Vaginitis is common among women of reproductive age and is usually characterized by vaginal discharge, vulvar itching and irritation, and a vaginal odor.[1] The three most common conditions diagnosed among women with vaginal symptoms presenting in the primary care setting are bacterial vaginosis (22 to 50%), trichomoniasis (4 to 35%), and vulvovaginal candidiasis (17 to 39%).[2] In some cases, the etiology of vaginitis may be mixed, and in approximately 30% of symptomatic women, no etiologic agent is identified.[3,4] The development of vaginitis is impacted by the dynamic vaginal ecosystem, which changes with age. The normal vaginal bacterial microbiota is dominated by Lactobacillus species, but a variety of other facultative and strict anaerobic bacteria are also present at much lower levels. Lactobacilli convert glycogen to lactic acid, which helps to maintain a normal acidic vaginal pH of 3.8 to 4.5. Some lactobacilli produce H2O2 (hydrogen peroxide), which serves as a host defense mechanism and kills bacteria and viruses. Normal vaginal discharge is clear to white, odorless, and of high viscosity. The following will address the most common causes of vaginitis is addressed in the individual sections in this lesson on Bacterial Vaginosis, Trichomoniasis, and Vulvovaginal Candidiasis.
- Module 2 Overview
Self-Study Lessons - 0%Lesson 1
Chlamydial InfectionsActivities- 0%Lesson 2
Gonococcal InfectionsActivities- 0%Lesson 3
SyphilisActivities- 0%Lesson 5
Genital HerpesActivities- 0%Lesson 6
Human Papillomavirus InfectionActivities- 0%Lesson 7
Pelvic Inflammatory DiseaseActivities- 0%Lesson 8
VaginitisActivities- 0%Lesson 9
MpoxActivities- 0%Lesson 10
Mycoplasma genitaliumActivitiesLesson 8. Vaginitis
PDF ShareLast Updated: March 20th, 2025Authors:David H. Spach, MD,David H. Spach, MD
Editor-in-Chief
Professor of Medicine
Division of Allergy and Infectious Diseases
University of WashingtonDisclosures: NoneChristina A. Muzny, MD, MSPH,Christina A. Muzny, MD, MSPH
Professor of Medicine, Epidemiology, and Obstetrics & Gynecology
Division of Infectious Diseases
University of Alabama at Birmingham
Teaching faculty, Southeast STD/HIV Prevention Training CenterDisclosures: Consulting Fee: Abbot, Biomerieux, BioNTech
Presentation Development: Elsevier
Lectures/Speaker Bureau: BD, CepheidRaaka G. Kumbhakar, MD, MPHRaaka G. Kumbhakar, MD
Assistant Professor of Medicine
Division of Allergy and Infectious Diseases
University of WashingtonDisclosures: NoneLearning Objective Performance Indicators
- Summarize the pathogenesis and microbiology for common infectious causes of vaginitis
- Recognize clinical manifestations of bacterial vaginosis, trichomoniasis, and vulvovaginal candidiasis
- Use recommended laboratory methods to diagnose bacterial vaginosis, trichomoniasis, or vulvovaginal candidiasis
- Provide recommended treatment for women with bacterial vaginosis, trichomoniasis, or vulvovaginal candidiasis
- Select appropriate vaginitis treatment regimens for pregnant women
Table of Contents- Vaginitis
- Introduction
- Diagnostic Approach for Vaginitis
- Bacterial Vaginosis
- Trichomoniasis
- Vulvovaginal Candidiasis
- Introduction
- Epidemiology
- Pathogenesis and Microbiology
- Factors Associated with Vulvovaginal Candidiasis
- Classification of Vulvovaginal Candidiasis
- Clinical Manifestations
- Diagnostic Methods
- Treatment of Uncomplicated Vulvovaginal Candidiasis
- Treatment of Complicated Vulvovaginal Candidiasis
- Counseling and Education
- Summary Points
- Check-On-Learning
- Citations
- Additional References
- Figures
- Tables
Introduction
Diagnostic Approach for Vaginitis
General Principles of Diagnosis
Vaginitis is primarily a clinical diagnosis, but a complete history, physical examination, and laboratory evaluation are necessary for accurate diagnosis. When evaluating a woman with vaginal symptoms, clinicians should inquire specifically about a woman’s menstrual cycle, sexual history (including sex partners and specific sexual practices), vaginal hygiene practices (such as douching), medication use (including any intravaginal products), and any other underlying medical conditions.[5] The following briefly addresses the general approach for evaluating vaginitis, including clinical evaluation and diagnostic testing options.
Clinical Evaluation
The evaluation of vaginitis requires visual inspection of the vaginal discharge, the vagina, and the cervix, as well as the collection and evaluation of a discharge specimen under the microscope. Visualization of the cervix is important in order to rule out cervicitis as a source of abnormal vaginal discharge. The following characteristics of the vaginal discharge should be noted during examination:
- Color
- Viscosity
- Adherence to vaginal walls
- Presence of odor
Diagnostic Methods for Initial Evaluation of Vaginitis
Most of the diagnostic methods at the initial evaluation of vaginitis are not organism-specific, but can provide valuable information when trying to diagnose the cause of vaginitis[2,3,6]. The following provides a summary of major diagnostic tests used in evaluating women with vaginitis.
- Saline Wet Mount: To perform a saline wet mount, begin by collecting a sample of vaginal fluid from the lateral wall of the vagina using a cotton-tipped swab. Next, place a drop of 0.9% saline on a glass slide. Last, mix the vaginal fluid sample with the saline on the slide. Alternatively, place the vaginal swab into a test tube (with less than 1 mL of saline), gently stir, and then extract a drop from the solution in the tube and place it onto a glass slide. With either method, carefully place a coverslip over the mixed solution on the slide and then immediately examine under a microscope at both low (10x) and high (40x) power. Scan the slide thoroughly for clue cells and for motile trichomonad organisms. Delays of more than 10 minutes in viewing the wet mount significantly reduce the chance of visualizing motile trichomonads. Visualizing large motile organisms (trichomonads) is diagnostic for trichomoniasis and observing greater than 20% clue cells per high-power field is one of the Amsel criteria for a clinical diagnosis of bacterial vaginosis.
- Potassium Hydroxide (KOH) Preparation and Whiff Test: To perform this test, collect a sample of vaginal fluid (using a cotton-tipped swab) from the lateral wall of the vagina, place the sample on a glass slide, and add several drops of a 10% KOH solution to the slide. Soon after applying the KOH, the slide should be brought near the nose to perform the whiff test; the presence of a strong amine “fishy” odor is considered a positive whiff test. A positive whiff test is also one of the Amsel criteria for a clinical diagnosis of bacterial vaginosis. After performing the whiff test, carefully place a coverslip over the preparation on the slide and immediately examine under a microscope at both low (10x) and high (40x) power. The KOH kills most of the cells and bacteria, but does not significantly impact the fungal organisms, thereby making it easier to visualize the presence of yeasts or pseudohyphae. Visualizing fungal organisms in a person who is symptomatic is consistent with a diagnosis of vulvovaginal candidiasis.
- Litmus Testing for pH of Vaginal Fluid: To determine the pH of the vaginal fluid, place a pH litmus paper on the wall of the vagina or directly in pooled vaginal secretions. The normal pH of the vagina is typically between 3.8 and 4.5. A pH greater than 4.5. An elevated vaginal pH occurs in the setting of bacterial vaginosis and trichomoniasis. It should be noted, however, that trichomoniasis may occur in the setting of an elevated or normal vaginal pH.
- Vaginal Gram Stain: Performing an initial Gram stain on a sample from the vagina can provide useful information in women with suspected bacterial vaginosis or vulvovaginal candidiasis. With bacterial vaginosis, the Nugent criteria is an established scoring system used for the microbiological evaluation of bacterial vaginosis on a vaginal Gram stain slide.[7] In addition, clue cells can be visible on the Gram stain. For women with vulvovaginal candidiasis, the Gram stain may show large, gram-positive staining yeasts and hyphae, but a wet mount KOH is preferred.[6,8] Trichomoniasis is not diagnosed on Gram stain of a vaginal specimen.
- Point-of-Care Organism-Specific Tests: In addition to point-of-care diagnostic methods that are not organism-specific (microscopy, pH determination, and the “whiff test”), other point-of-care tests have been developed that are organism-specific and have good sensitivity and specificity.[3]
- Culture: Vaginal cultures can be performed for both T. vaginalis and Candida species. Fungal culture is not usually necessary to make a diagnosis of vulvovaginal candidiasis but may be needed in cases of recurrent vulvovaginal candidiasis or treatment failure with suspected azole resistance. For the diagnosis of T. vaginalis, culture for T. vaginalis is more sensitive than a wet mount, but less sensitive than molecular diagnostic methods, such as nucleic acid amplification testing.[9,10] Vaginal T. vaginalis culture may be needed in cases of persistent trichomoniasis so that antimicrobial resistance testing may be performed on the trichomonas isolate. Vaginal culture for bacterial vaginosis is not recommended due to low sensitivity (less than 50%) and the potential for mistakenly identifying commensal bacteria as pathogens, resulting in inappropriate treatment.[3]
- Nucleic Acid Amplification Tests (NAAT): There are multiple nucleic acid amplification tests (NAATs) that are available and FDA-cleared for the diagnosis of bacterial vaginosis, trichomoniasis, and candida vulvovaginal candidiasis.[10,11,12,13] Most of these NAATs utilize polymerase chain reaction (PCR)-based technology.
Bacterial Vaginosis
Introduction
Bacterial vaginosis (BV) is a condition characterized by alterations in the normal vaginal microbiota, with a loss of protective lactic-acid producing Lactobacillus species in conjunction with increases in the concentration of facultative and strict anaerobic bacteria.[14,15] Bacterial vaginosis can increase the risk of acquiring a number of sexually transmitted infections (STIs), including HIV.[14,16] Further, bacterial vaginosis may contribute to adverse birth outcomes, such as premature birth, low birth weight, and premature rupture of membranes.[17]
Epidemiology
Bacterial vaginosis is the most common cause of vaginal discharge among reproductive-aged women in the United States and worldwide.[2,18,19,20] The estimated prevalence of bacterial vaginosis among reproductive-aged women in the United States has ranged from a low of 17% to a high of 47%, with an overall estimated prevalence of approximately 25 to 30%.[18,20,21] In these studies, many of the women with bacterial vaginosis were asymptomatic. Since bacterial vaginosis is not a reportable infection, data on the prevalence and prevalence trends are limited, with estimates based on published studies. Data on the incidence of bacterial vaginosis are extremely limited. In North America alone, the estimated annual economic burden of treating symptomatic bacterial vaginosis is $1.3 billion, with a global economic burden of $4.8 billion.[20] When taking into account all sequelae associated with bacterial vaginosis, this attributable annual cost in North America increases to approximately $3.7 billion.[20]
Factors Associated with Increased Prevalence
Increased bacterial vaginosis prevalence is associated with a greater number of male sex partners, sex with a female partner, douching, and herpes simplex virus type 2 (HSV-2) infection (Figure 1).[18,19,22,23,24] A reduced risk is associated with consistent condom use, male partners who are circumcised, and oral contraceptive pills.[25,26] Increasing evidence suggests that sexual activity is integral to the development of incident bacterial vaginosis in most persons, as it correlates with the frequency of sexual activity, younger age at sexual debut, participating in anal and oral sex, and use of vaginal sex toys.[21,27,28,29,30,31] A recent study showing a significant reduction in recurrent bacterial vaginosis when regular male sex partners are treated with twice-daily oral metronidazole and topical clindamycin (applied to the penis glans and upper shaft), each for 7 days, has further strengthened the belief that sexual transmission of bacterial vaginosis–associated bacteria plays a key role in women developing bacterial vaginosis.[32,33] The role of sexual activity in bacterial vaginosis is also supported by indirect evidence, including (1) the absence of BV in women prior to sexual debut, (2) concordant vaginal flora among women in same-sex partnerships, and (3) elevated rates of bacterial vaginosis-associated bacterial colonization (as measured with penile swabs) among men engaging in extramarital sexual relationships, as compared with men who are monogamous.[30,34,35,36,37]
Pathogenesis and Microbiology
Current understanding of the pathogenesis of bacterial vaginosis suggests loss of normal Lactobacillus species in the vagina by multiple facultative and strict anaerobic bacteria, which subsequently leads to vaginal dysbiosis and a proinflammatory state.[14,16,38] To date, however, the exact etiology of bacterial vaginosis has not been determined, despite extensive research. The following summarizes current step-by-step conceptual models for the pathogenesis of bacterial vaginosis.[14,16,39]
- In the baseline state in a healthy vaginal microbiome, protective Lactobacillus species are dominant, and they produce lactic acid from glycogen, a process that maintains a low vaginal pH; this acidic pH environment inhibits the growth of other bacterial species that are normally present in the vagina at very low levels.
- The process of vaginal dysbiosis usually begins with the colonization of the vagina by a virulent strain of Gardnerella species, typically following sexual exposure; the proliferation of this organism displaces vaginal lactobacilli and creates a biofilm scaffolding conducive to recruiting Prevotella bivia (and other BV-associated bacteria).[40,41]
- Gardnerella species and P. bivia engage in a synergistic relationship in which proteolysis by Gardnerella species produces amino acids that enhance the growth of P. bivia. In turn, ammonia produced by P. bivia enhances the growth of Gardnerella species.
- Sialidase, produced by both P. bivia and Gardnerella species, promotes the breakdown of the mucin layer of the vaginal epithelium and increases adherence of other strict anaerobes, including Fannyhesseae vaginae, Sneathia species, Megasphaera type I, and others which join the BV biofilm on the upper layers.
- Fannyhesseae vaginae stimulates a strong host immune response from vaginal epithelial cells, leading to localized cytokine and beta-defensin production.
- Gradually, the healthy normal dominant vaginal lactobacilli are replaced by Gardnerella species, F. vaginae, bacterial vaginosis-associated bacteria-2 (BVAB-2), Sneathia species, Megasphaera type I, and other BV-associated bacteria.
- In the final phase of this transition to bacterial vaginosis, mucus degradation occurs, the vaginal pH is elevated, and multiple harmful compounds are produced (biogenic amines, toxic metabolites, and proinflammatory cytokines)—all resulting in a final state of vaginal dysbiosis and inflammation, which may progress to cause vaginal symptoms and adverse outcomes associated with this infection.[16]
Watch this 6-minute illustrated video by Dr. Christina A. Muzny on the pathogenesis of bacterial vaginosis.Clinical Manifestations
Among women with bacterial vaginosis, approximately 50 to 75% are asymptomatic.[18,42] If symptomatic, most women with bacterial vaginosis will describe vaginal malodor and vaginal discharge.[43] The odor is often described as an unpleasant “fishy smell” that may become more prominent after sexual intercourse and around the time of menstruation; the discharge is typically off-white, thin, and homogeneous.[3,38,44] Symptoms may remit spontaneously. Bacterial vaginosis does not typically cause pruritus, burning, dysuria, dyspareunia, vaginal inflammation, or vulvar swelling.[44] Qualitative studies have shown that bacterial vaginosis can negatively impact self-esteem, sexual relationships, and quality of life.[21,28,45]
Obstetrical and Gynecologic Complications
Bacterial vaginosis has been linked to several obstetric complications, including late miscarriage, premature rupture of membranes, premature delivery, and low birth weight at delivery.[17,46,47,48] Bacterial vaginosis has also been associated with gynecologic complications, particularly an increased risk of post-operation infections after gynecological procedures.[49,50] There are some data to suggest bacterial vaginosis may cause additional gynecologic complications, including endometritis, pelvic inflammatory disease, and infertility, but prospective, longitudinal studies are needed to conclusively determine if bacterial vaginosis clearly causes these complications.[51,52]
Impact on Acquisition and Transmission of STIs
Longitudinal studies have also shown that bacterial vaginosis confers a substantially increased risk of acquiring multiple bacterial and viral STIs, including chlamydia, gonorrhea, trichomonas, Mycoplasma genitalium, herpes simplex virus type 2, human papillomavirus, and HIV.[53,54,55,56,57,58] Investigators have shown that disruptions of vaginal microbiota with bacterial vaginosis result in high concentrations of specific vaginal bacteria that increase the risk of HIV acquisition in women.[59] The increased risk for HIV acquisition from bacterial vaginosis is thought to occur from the altered bacterial microflora environment, causing genital inflammation, impaired vaginal wound healing, and disruptions in the integrity of the mucosal barrier.[60] Additional studies have also shown that bacterial vaginosis increases genital HIV-1 shedding in women and enhances the risk of female-to-male HIV-1 transmission.[61]
Diagnostic Approach
Gram staining of a vaginal specimen with Nugent scoring has traditionally been considered the gold standard for diagnosing bacterial vaginosis, but it is primarily used only in research settings. In the clinical setting, point-of-care testing, such as the Amsel criteria and OSOM BVBlue test, are the most frequently used tests for diagnosing bacterial vaginosis. In addition, in recent years, molecular assays have emerged to play an increasingly important role in the diagnosis of bacterial vaginosis. Specimens for molecular testing should only be obtained from symptomatic women.[62,63] Making a diagnosis of bacterial vaginosis with vaginal culture or by examining a Papanicolaou smear (Pap test) is not recommended due to low sensitivity and specificity.[64,65,66]
Amsel Criteria
Bacterial vaginosis is most commonly diagnosed clinically using the Amsel criteria.[67] Compared with the traditional gold standard (vaginal fluid Gram stain with Nugent scoring), the Amsel criteria have a sensitivity in the range of 37 to 70% and specificity of 94 to 99%.[12] In the Amsel criteria, The presence of three of the following four criteria provides sufficient evidence for a clinical diagnosis of bacterial vaginosis:[43,68]
- Vaginal pH greater than 4.5, which is the most sensitive but least specific sign
- Positive amine, “whiff” or “fishy odor” test (liberation of biologic amines with or without the addition of 10% KOH)
- Homogeneous, nonviscous, milky-white discharge adherent to the vaginal walls
- The presence of “clue cells” (bacterial clumping that obscures the borders of vaginal epithelial cells) (Figure 2) in at least 20% of vaginal epithelial cells per high-power field viewed on saline microscopy
Vaginal Gram Stain with Nugent Scoring
The traditional gold standard for diagnosing bacterial vaginosis is a vaginal Gram stain with Nugent score determination, which is based on the relative concentration of Lactobacillus, Bacteroides, Gardnerella, and Mobiluncus species (Figure 3).[7,63] A normal Gram stain should show Lactobacillus species only or Lactobacillus species with only a few Gardnerella morphotypes; a Nugent score of 0 to 3 is considered normal and is consistent with a Lactobacillus-predominant vaginal microbiota, a score of 4 to 6 indicates intermediate microbiota (emergence of G. vaginalis), and 7 to 10 is consistent with bacterial vaginosis.[7,63] Although this test is traditionally considered the gold standard, it is not used often in clinical practice because it is time-consuming, requires training and expertise for interpretation, and results are not typically available during a clinic visit.[12]
Point-of-Care Assays
In addition to the point-of-care methods used to determine the Amsel criteria, several assays have been developed as point-of-care tests for the diagnosis of bacterial vaginosis.
- OSOM BVBlue Test: The OSOM BVBlue test detects elevated vaginal fluid sialidase, an enzyme that is produced in increased quantities by certain bacterial microorganisms (i.e., G. vaginalis) that are involved in bacterial vaginosis.[69,70] This test is a Clinical Laboratory Improvement Amendments (CLIA)-waived, point-of-care test that provides results in about 10 minutes.[12] The test is easy to perform and requires six steps: (1) obtain a vaginal swab sample using the kit swab (either through self-collected or clinician-collected specimens), (2) insert the collection swab into the kit testing vial that contains liquid, (3) wait 10 minutes with the swab in the vial, (4) add one drop of the developer solution to the testing vessel, (5) stir the swab in the vial to mix the test solution with the vial solution, and (6) immediately read the test and interpret based on the color change. Compared with a Nugent score, this test has a sensitivity in the range of 88 to 92% and a specific range of 92-95%.[69,70]
- Affirm VPIII: This molecular assay uses a DNA hybridization probe that can detect high concentrations of G. vaginalis (greater than 5 × 105 colony-forming units of G. vaginalis per mL of vaginal fluid); this assay can also detect T. vaginalis and C. albicans. The test requires approximately 30 minutes to obtain results. When the Affirm VPIII assay is used alone to diagnose bacterial vaginosis, it has a low sensitivity and specificity when compared with a Gram stain and Nugent scoring. If, however, this test is used in conjunction with a vaginal pH measurement and the presence of amine odor, the test performance improves, with a sensitivity of 97% and specificity of 81%.[12]
- FemExam Test Card: The FemExam Test Card measures vaginal pH, proline aminopeptidase, and trimethylamine (a metabolic by-product of G. vaginalis).[71] When compared with a Gram stain and Nugent score, this test has a sensitivity of 91% and specificity of 61%.[63] This test has primarily been used in resource-limited settings, and although it has been reported to be beneficial compared with syndromic management, it is not a preferred diagnosis method for bacterial vaginosis.[62,71]
Nucleic Acid Amplification Tests
Although multiple nucleic acid amplification tests (NAATs) are commercially available for diagnosing bacterial vaginosis in symptomatic women, only three of these are cleared by the United States Food and Drug Administration (FDA): BD MAX Vaginal Panel, Aptima BV, and GeneXpert Xpress MVP.[12,63] These tests are currently intended only for use in women with vaginitis symptoms, and can be run using a self-obtained or clinician-collected vaginal swab specimens, with results available within 24 hours.[12,62]
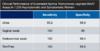
- BD MAX Vaginal Panel: The BD MAX Vaginal Panel is a multiplex, real-time PCR assay used to evaluate women with vaginitis symptoms. This assay can detect major Lactobacillus species that are present in a healthy vaginal microbiota (L. crispatus, L. gasseri, and L. jensenii) and prominent bacterial vaginosis-associated bacteria (G. vaginalis, A. vaginae, BVAB-2, and Megasphaera type 1).[63,72] In addition, the BD MAX Vaginal Panel can detect organisms responsible for causing trichomoniasis and vulvovaginal candidiasis.[72] This assay bases the diagnosis of bacterial vaginosis on the relative concentrations of the healthy Lactobacillus species and the bacterial vaginosis-causing organisms, with a final determination based on a proprietary algorithm.[63] For the diagnosis of bacterial vaginosis, this test has a reported sensitivity with clinician-collected specimens of 90.5% and specificity of 85.8%; similar results were seen with self-obtained specimens (Figure 4).[72]
- Aptima BV Test: The Aptima BV test can be used in symptomatic women to detect certain Lactobacillus species (L. crispatus, L. gasseri, and L. jensenii) and bacterial vaginosis-associated bacteria (G. vaginalis and A. vaginae). This test has a reported sensitivity with clinician-collected specimens of 95.0% and specificity of 89.6%; similar results were seen with self-obtained specimens (Figure 5).[73]
- Gene Xpert Xpress MVP: The Xpert Xpress MVP is a Clinical Laboratory Improvement Amendments (CLIA)-waived, on-demand diagnostic PCR test which detects DNA targets from anaerobic bacteria associated with BV (F. vaginae, BVAB-2, Megasphaera type 1), Candida species, and T. vaginalis. For bacterial vaginosis, as compared to the BD MAX Vaginal Panel, the MVP test demonstrated high positive and negative percent agreement for both clinic and self-collected specimens (93.6-99% and 92.1%-99.8%, respectively).[74]
Screening Recommendations
In general, screening for bacterial vaginosis in asymptomatic women is not recommended. Screening and treatment of women with bacterial vaginosis prior to a surgical abortion or hysterectomy can be considered due to decreased rates of postsurgical infections in women pretreated with metronidazole; cost-comparison studies have found that adding metronidazole to standard surgical prophylaxis is more cost-effective than a screen-and-treat approach.[75,76,77,78] Despite a link between bacterial vaginosis and preterm birth, several studies have concluded that treatment of bacterial vaginosis does not reduce the likelihood of preterm birth.[79,80,83] For pregnant women who do not have vaginal symptoms, routine screening for bacterial vaginosis is not recommended, including women at low risk or high risk for preterm delivery.[63]
Treatment
Treatment of Bacterial Vaginosis in Nonpregnant Women
Women who have vaginal symptoms consistent with bacterial vaginosis should receive treatment.[63] The recommended regimens include metronidazole 500 mg orally twice daily for 7 days; metronidazole 0.75% gel, 5 grams intravaginally once a day for 5 days; or clindamycin 2% cream, 5 grams intravaginally at bedtime for 7 days (see Table 1 below).[63] Accumulating reports have refuted prior warnings that metronidazole (or tinidazole) causes a disulfiram-like reaction in persons who ingest alcohol while taking these antibiotics.[84,85] Accordingly, experts now consider it unnecessary for persons to refrain from ingesting alcohol when they are taking metronidazole or tinidazole.[63,85] Secnidazole is a newer nitroimidazole that has been FDA-approved as a 2-gram single-dose packet for the treatment of bacterial vaginosis for females who are 12 years of age and older.[86,87] Although the use of probiotics that target vaginal repletion of Lactobacillus species is an attractive concept for treatment and for prevention of recurrences of bacterial vaginosis, this strategy is not recommended at this time.[63,88,89,90]
Table 1. 2021 STI Treatment Guidelines: Bacterial VaginosisTreatment of Bacterial VaginosisRecommended RegimensMetronidazole500 mg orally twice a day for 7 daysMetronidazole
Tradename:FlagylRecommended RegimensMetronidazole gel 0.75%one full applicator (5 g) intravaginally, once a day for 5 daysMetronidazole gel 0.75%
Tradename:Recommended RegimensClindamycin vaginal cream 2%one full applicator (5 g) intravaginally at bedtime for 7 daysClindamycin vaginal cream 2%
Tradename:Cleocin vaginal creamNote: Clindamycin cream is oil based and might weaken latex condoms and diaphragms for 5 days after use.Alternative RegimensClindamycin300 mg orally twice daily for 7 daysClindamycin
Tradename:CleocinAlternative RegimensClindamycin ovules100 mg intravaginally once at bedtime for 3 daysClindamycin ovules
Tradename:Note: Clindamycin ovules use an oleaginous base that might weaken latex or rubber products (e.g. condoms and diaphragms). Use of such products within 72 hours after treatment with clindamycin ovules is not recommended.Alternative RegimensSecnidazole2 g oral granules in a single doseSecnidazole
Tradename:SolosecNote: Oral granules should be sprinkled onto unsweetened applesauce, yogurt, or pudding before ingestion. A glass of water can be taken after administration to aid in swallowing.Alternative RegimensTinidazole2 g orally once daily for 2 daysTinidazole
Tradename:TindamaxAlternative RegimensTinidazole1 g orally once daily for 5 daysTinidazole
Tradename:TindamaxSource: Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. Diseases characterized by vaginal itching, burning, irritation, odor or discharge: bacterial vaginosis. MMWR Recomm Rep. 2021;70(No. RR-4):1-187. [2021 STI Treatment Guidelines]Management of Sex Partners
Current CDC guidelines do not recommend routine testing or treatment of male or female sex partners of women diagnosed with bacterial vaginosis.[63]
- Management of Male Sex Partners: The current recommendation for the management of male sex partners of women diagnosed with bacterial vaginosis is likely to change based on a recently published trial from Australia that showed a significant benefit in reducing recurrent bacterial vaginosis when treating male partners with oral metronidazole and clindamycin cream (applied to the penis glans and upper shaft).[33,37] In this trial, investigators enrolled premenopausal women diagnosed with bacterial vaginosis who were in a monogamous relationship with a male partner and randomized the male sex partners to receive treatment for bacterial vaginosis or placebo.[32] A total of 164 heterosexual couples were enrolled.[32] Women with bacterial vaginosis were treated with a first-line regimen and male partners randomized to treatment received oral metronidazole 400 mg twice daily for 7 days and topical 2% clindamycin cream applied to the glans penis and upper shaft for 7 days.[32] The primary outcome measure was recurrent bacterial vaginosis within 12 weeks of receiving treatment. Among the 137 couples who completed the trial, recurrent bacterial vaginosis occurred in 24 of 69 (35%) of women in the partner-treatment group, compared with 43 of 68 (63%) of women in the partner-placebo group (P<0.001).[32] Of note, the trial was stopped early because of the superiority of the primary outcome in the male partner treatment group.[32] Experts have noted that findings from this study support the role of sexual transmission of bacterial vaginosis-associated bacteria, likely leading to a new approach that involves routinely treating male sex partners of women diagnosed with bacterial vaginosis.[33]
- Management of Female Sex Partners: Data for the treatment of female partners of women diagnosed with bacterial vaginosis are limited. Because female sex partners are often concurrent with bacterial vaginosis status, the option of screening and treatment of female sex partners could be considered, but this approach has not been studied rigorously in clinical trials.[91]
Post-Treatment Follow-Up
Follow-up after treatment of bacterial vaginosis is only necessary if symptoms persist or recur.[63]
Special Considerations
The following situations require unique consideration when treating bacterial vaginosis.
- Metronidazole (or Tinidazole) Allergy or Intolerance: For women who are allergic or intolerant to metronidazole (or tinidazole), the preferred option is to treat with clindamycin cream using one full applicator (5 grams) intravaginally at bedtime for 7 days.[63]
- Treatment of Symptomatic Bacterial Vaginosis in Pregnancy: All pregnant women who have symptomatic bacterial vaginosis should receive treatment since symptomatic bacterial vaginosis is clearly associated with adverse pregnancy outcomes.[63] Further, treating symptomatic bacterial vaginosis in pregnancy reduces symptoms and may reduce certain adverse obstetrical outcomes, such as late miscarriage. Any of the recommended bacterial vaginosis treatments for nonpregnant women (oral metronidazole, metronidazole gel, and clindamycin cream), as well as certain alternative regimens (oral clindamycin and clindamycin ovules), can be used to treat symptomatic bacterial vaginosis during pregnancy. Metronidazole crosses the placenta and is excreted in breast milk, but it has not been linked to teratogenic effects.[92,93,94] Tinidazole is not recommended during pregnancy due to evidence of fetal harm in animal studies. There are insufficient data in pregnancy to recommend using secnidazole in pregnant women with bacterial vaginosis.[95,96,97] Several additional preparations should not be used during pregnancy, including metronidazole 1.3% vaginal gel, the 750-mg vaginal metronidazole tablets, and the Clindesse brand of 2% clindamycin vaginal cream, which is a high-dose single-application treatment for bacterial vaginosis. For breastfeeding mothers with symptomatic bacterial vaginosis, oral metronidazole can be used.[63]
- Management of Asymptomatic Bacterial Vaginosis in Pregnancy: Since routine screening for bacterial vaginosis is not recommended for pregnant women who do not have vaginal symptoms, the need to address the treatment of asymptomatic bacterial vaginosis during pregnancy should not routinely arise. Available data suggest no benefit for the treatment of asymptomatic bacterial vaginosis in pregnant women who are considered at low risk for preterm delivery.[98] For pregnant women at high risk for preterm delivery, the impact of treating asymptomatic bacterial vaginosis is not clear, and available data are conflicting: four studies showed benefit with treatment, two showed no benefit, and one showed harm.[63]
- Treatment in Women with HIV: Women with HIV experience higher prevalence and longer persistence of bacterial vaginosis compared to women without HIV.[99] The treatment of bacterial vaginosis in women with HIV should be the same as for women without HIV.[63]
Treatment of Recurrent Bacterial Vaginosis
Bacterial vaginosis recurs in approximately 30% of women within the first 3 months following treatment and in up to 50% of women after 6 to 12 months.[100,101] Very little is known about antimicrobial resistance with pathogens that cause bacterial vaginosis, although clinical experience suggests that treatment failure from true antimicrobial resistance is uncommon.[28,102]- Single Recurrence: Women with a single recurrence can be treated with either the same recommended regimen or a different recommended regimen.[63,103]
- Multiple Recurrences: For women who experience multiple recurrences of bacterial vaginosis after completing treatment with a recommended regimen, a different approach from the initial treatment should be utilized.[102] Suggested interventions include switching the route of therapy (from oral to vaginal or vice versa) or switching the class of drug.[102,104] Based on available data, the following alternative regimens are suggested as options for these women.[63]
- Metronidazole gel (0.75%) vaginal suppository twice-weekly for at least 3 months.[101]
- Metronidazole 750 mg vaginal suppository twice-weekly for at least 3 months.[105]
- Metronidazole 500 mg orally twice daily (or tinidazole 500 mg orally twice daily) for 7 days, followed by intravaginal boric acid 600 mg daily for 21 days, followed by suppressive therapy with intravaginal metronidazole gel (0.75%) twice-weekly for 4 to 6 months.[106]
- Metronidazole 2 grams orally once per month plus fluconazole 150 mg orally once per month given over a 12-month timeframe has also been evaluated as periodic presumptive therapy; this approach resulted in fewer episodes of bacterial vaginosis in one study when compared to placebo.[107]
- Astodrimer 1% gel (a dendrimer-based microbicide) at a dose of 5 grams vaginally every other day for 16 weeks.[108]
- Treatment of Male Sex Partners: Although not yet recommended as an approach in CDC guidelines, new data have shown that treatment of male sex partners with oral metronidazole and topical clindamycin cream (applied to penis glans and upper shaft) markedly reduces the incidence of recurrent bacterial vaginosis in women.[32] Thus, treatment of male sex partners should now be considered for the prevention and management of recurrent bacterial vaginosis in women.[33]
Counseling and Education
Patient counseling and education about bacterial vaginosis should cover the nature of the disease and transmission issues.
Nature of the Disease
- Asymptomatic bacterial vaginosis is common, and screening of asymptomatic women is not generally recommended.
- Bacterial vaginosis is caused by a shift in the normal vaginal flora microbiota from lactobacillus predominance to a predominance of facultative and strict anaerobic bacteria.
- The hallmark of symptomatic bacterial vaginosis is vaginal malodor and discharge.
- Bacterial vaginosis is associated with multiple obstetric and gynecologic complications, including preterm birth and pelvic inflammatory disease, and it is associated with an increased risk of acquisition of HIV and other STIs.
Transmission Issues
- Sexual activity is significantly implicated in the pathogenesis of incident bacterial vaginosis; sexual transmission of bacterial vaginosis-associated bacteria is highly likely.
- The pathogenesis of recurrent and persistent bacterial vaginosis may be different from incident bacterial vaginosis.
- There is a high concordance for the presence or absence of bacterial vaginosis in partnerships involving women who have sex with women.
- Bacterial vaginosis increases a woman’s risk of acquiring sexually transmitted infections (STIs), including chlamydia, gonorrhea, genital herpes, and HIV.
- Women with HIV and bacterial vaginosis have a higher likelihood of transmitting HIV to their sex partners.
Trichomoniasis
Introduction
Trichomoniasis is caused by the protozoan parasite Trichomonas vaginalis and is the most common curable STI worldwide. Clinical manifestations associated with trichomoniasis include asymptomatic infection, acute infection, and chronic vaginitis.[109,110] Trichomoniasis in pregnancy has been associated with obstetrical and gynecologic adverse outcomes.[111,112] A meta-analysis of 17 published studies found that women with T. vaginalis were at a two-fold higher risk for developing cervical cancer.[113] In addition to these clinical complications, trichomoniasis also confers a two- to three-fold risk of acquiring HIV.[114,115,116]Epidemiology
An estimated 3.7 million people have trichomoniasis in the United States, with approximately 1.1 million new cases occurring each year.[117,118,119] The prevalence of T. vaginalis infection among women of reproductive age in the United States is estimated at 2.1%, but rates are at least four times higher among non-Hispanic Black women.[120] In contrast to chlamydia and gonorrhea, which have the highest rates in women younger than age 25 years, the prevalence of T. vaginalis is lower in women younger than 20 years of age than in women 20 to 50 years of age (Figure 6).[121] Prevalence rates are significantly higher in women with vaginal symptoms: in one study of women attending sexually transmitted diseases (STD) clinics, the trichomonas prevalence was 26.2% among symptomatic women compared to 6.5% among asymptomatic women.[122] Although men are not routinely tested for trichomoniasis, studies have reported rates from 3 to 17% in men attending STI clinics and as high as 72% among men who have female sex partners diagnosed with trichomoniasis.[123,124,125] Men who have sex with men appear to be at low risk of acquiring trichomoniasis.[126] Transmission of T. vaginalis between women who have sex with women has been documented to occur at a substantial rate.[127,128]
Pathogenesis and Microbiology
The etiologic agent in trichomoniasis is T. vaginalis, which is a single-celled flagellated anaerobic protozoan parasite. It is the only known protozoan parasite that infects the genital tract. Trichomonas vaginalis has four anterior flagella and one flagellum embedded in an undulating membrane (Figure 7).[110] The flagella are responsible for the jerky motility of this organism that is seen under a microscope. After attaching to vaginal epithelial cells, this globular, pear-shaped organism transforms into a thin, flat, ameboid shape.[129] Trichomoniasis is almost always sexually transmitted. Trichomonas vaginalis may persist for months to years in epithelial crypts and periglandular areas of the genital tract.[110] Distinguishing persistent, subclinical infection from remote sexual acquisition is not always possible.
Factors Associated with Increased Prevalence
Investigators have identified multiple factors associated with trichomoniasis, including current or past incarceration, two or more sex partners in the prior year, a diagnosis of bacterial vaginosis, education less than completion of high school, and living below the national poverty level.[130,131,132,133]
Clinical Manifestations
Genitourinary Infection in Women
Vaginitis due to acute infection with T. vaginalis can have a characteristic “frothy” gray or yellow-green vaginal discharge and pruritus, but many women are asymptomatic. On pelvic examination, the presence of cervical punctate hemorrhages, often referred to as a “strawberry cervix,” strongly suggests a diagnosis of trichomoniasis, but this occurs in fewer than 5% of women with trichomoniasis (Figure 8).[110] Chronic infection may be associated with minimal vaginal discharge, mild pruritus, and/or dyspareunia.[110,134] Infection with T. vaginalis has also been associated with an increased risk of infertility, PID, and cervical cancer.[113,135,136]
Trichomoniasis in Pregnancy
Infection with T. vaginalis in pregnant women is associated with both obstetrical and gynecologic adverse outcomes, including premature rupture of membranes and preterm labor; trichomoniasis in pregnancy increases the risk of preterm birth by about 30%.[111,112,137,138] Neonatal trichomoniasis is unusual but can occur.[139,140]
Trichomoniasis in Persons with HIV
Among women with HIV, more than half are coinfected with T. vaginalis, and they have been shown to have an increased risk for pelvic inflammatory disease and for shedding of HIV in the genital tract.[141,142,143,144] Antiretroviral therapy appears to lessen the potentiating effects of trichomoniasis infections on HIV transmission risk.[144] Infection with HIV does not make a woman more likely to have persistent or recurrent trichomoniasis.[145]
Trichomoniasis in Men
Trichomonas vaginalis may cause up to 11 to 13% of nongonococcal urethritis (NGU) in men, but urethral infection in men is frequently asymptomatic.[146] Men with T. vaginalis infection may also rarely present with prostatitis or epididymitis.[147] Infection with T. vaginalis in men may also contribute to impaired sperm motility.
Diagnostic Methods
Diagnostic testing for trichomoniasis should be performed in women seeking evaluation of vaginal discharge.[147] In clinical practice, wet mount preparation has been the most commonly used method for diagnosing trichomoniasis, primarily because of the low cost, convenience, and point-of-care diagnosis.[9,10] This approach, however, has a sensitivity (44 to 68%) that is significantly lower than with newer molecular NAATs.[13] Papanicolaou testing is not considered an appropriate diagnostic tool for trichomoniasis; if T. vaginalis infection is identified on routine Papanicolaou testing, a standard trichomonas diagnostic test should be used to verify infection. The following summarizes the major methods used to diagnose trichomoniasis.
Wet Mount Preparation
In the clinical setting, the diagnosis of trichomoniasis can be made by microscopic visualization of motile trichomonads on a vaginal wet mount slide (Figure 9).[9,148] Although the wet mount method is inexpensive and relatively simple to perform, it has a sensitivity of only 44 to 68%, and it is operator-dependent.[9] Once a vaginal fluid sample is collected, it should be stored in saline (for a maximum of one hour) until the operator is ready to perform microscopy.[149] Once the specimen has been placed on the slide, microscopic evaluation is recommended as soon as possible and always within 10 minutes, since the trichomonads will become increasingly sluggish on the wet mount, and motility is required for positive identification.[9,148,149]
Culture
Obtaining a culture using modified Diamond’s medium was the previous gold standard for diagnosis of trichomoniasis prior to the availability of highly sensitive NAATs. Culture is a more sensitive diagnostic tool than wet mount alone, but results are not immediately available. Specialized culture systems (i.e., InPouch System [Biomed Diagnostics]) are available to allow for transport of cultures when shipping to an off-site laboratory. Culture may be used for diagnosing T. vaginalis in both men and women. Culture in men may be performed on samples of urethral secretions, urine sediment, or semen, but testing in women requires sampling of vaginal secretions, as the sensitivity is low in urine culture.[147] Trichomonas vaginalis culture is categorized by the Clinical Laboratory Improvement Amendments (CLIA) as moderately complex as it is time-consuming and requires incubation.[13] If T. vaginalis is isolated in culture, drug susceptibility testing can be performed, particularly in cases of persistent infection.
Nucleic Acid Amplification Testing (NAAT)
Several NAAT-based methods are available for the diagnosis of T. vaginalis, including transcription-mediated amplification and polymerase chain reaction (PCR). There are no data to suggest T. vaginalis causes oral or anorectal infection, and therefore use of NAAT to detect T. vaginalis oral or anorectal infection is not recommended.[147,150,151]
- Aptima Trichomonas vaginalis Assay (Becton Dickinson [BD]): This assay uses transcription-mediated amplification for the detection of T. vaginalis RNA.[146,152] This test is FDA-cleared for detectingT. vaginalis in symptomatic and asymptomatic women.[147] The test can be performed on clinician-collected vaginal swabs, clinician-collected endocervical swabs, female urine specimens, or liquid endocervical Pap smear specimens collected in PreservCyt Solution.[146,153] The Aptima Trichomonas vaginalis assay has a sensitivity of 95.3 to 100% and specificity of 95.2 to 100%, which are considerably higher than wet mount or culture (Figure 10).[146,154,155,156] The Aptima Trichomonas vaginalis assay is not FDA-cleared for use in men, but it may be used to test urine or urethral swabs from men if the assay is internally validated in accordance with CLIA regulations.[147]
- Probe Tec TV Qx Amplified DNA Assay (Becton Dickinson [BD]): This assay uses Strand Displacement Amplification technology and is FDA-cleared for detection of T. vaginalis from vaginal swabs (clinician-collected or self-collected), endocervical swabs (clinician-collected), and female urine specimens.[147] This assay can be used to detect T. vaginalis in symptomatic and asymptomatic females. The Probe Tec TV Qx Amplified DNA assay has a sensitivity of 98.3% and specificity of 99.6% for detecting T. vaginalis.[157]
- GeneXpert TV (Cepheid): This PCR-based NAAT is FDA-cleared for the detection of T. vaginalis genomic DNA using self-collected or clinician-collected vaginal specimens, female urine specimens, clinician-collected endocervical swab specimens, and male urine specimens.[147,158] With this assay, the results are available within 63 minutes; for samples that have a clear positive result after 45 PCR cycles have been completed, the Early Assay Termination function will provide the positive result earlier, typically within 40 minutes.[158] The GeneXpert TV has a sensitivity of 99.5 to 100% and a specificity of 99.4 to 99.9%.[72]
- Gene Xpert Xpress MVP (Cepheid): The Xpert Xpress MVP is a CLIA-waived on-demand diagnostic PCR test that detects DNA targets from T. vaginalis as well as Candida species and anaerobic bacteria associated with BV (F. vaginae, BVAB-2, Megasphaera type 1.[74]
- Max CTGCTV2 Assay (Becton Dickinson): This test is an FDA-cleared PCR assay for detecting Chlamydia trachomatis, Neisseria gonorrhoeae, and T. vaginalis from vaginal specimens (self-collected or clinician-collected), female urine specimens, and male urine specimens.[147,159] The Max CTGCTV2 Assay has a sensitivity of 96.2-100% and a specificity of 99.1-100% for detecting T. vaginalis.[72]
- Cobas TV/MG (Roche Diagnostics): This PCR-based NAAT is FDA-cleared for the detection of T. vaginalis and M. genitalium using vaginal specimens (self-collected or clinician-collected), clinician-collected endocervical swab specimens, female urine specimens, male urine specimens, and clinician-collected meatal specimens.[160] This assay is FDA-cleared for both symptomatic and asymptomatic patients. The Cobas TV/MG has a sensitivity and specificity greater than 99.5%.[160,161]
- Alinity m STI Assay (Abbott): The Alinity m STI assay is an in vitro reverse transcription-polymerase chain reaction (RT-PCR) assay that is FDA-cleared for the detection of four common STIs: C. trachomatis, N. gonorrhoeae, T. vaginalis, and M. genitalium. This assay may be used on clinician or self-collected vaginal swab specimens, endocervical swab specimens, gynecological specimens collected in ThinPrep PreservCyt solution, and female and male urine specimens from asymptomatic and symptomatic individuals.[162] In a recent study, the overall percent agreements of the Alinity m STI assay in comparison with the Aptima and cobas assays for the four organisms tested were: C. trachomatis (99.5% [97.2%, 99.9%]), N. gonorrhoeae (99.5% [97.2%, 99.9%]), T. vaginalis (98.4% [95.5%, 99.5%]), and M. genitalium (86.4% (66.7%, 95.3).[163]
Point-of-Care Testing
There are multiple point-of-care tests available for diagnosing trichomoniasis in women.[164]
- Osom Trichomonas Rapid Test (Sekisui Diagnostics): This is an antigen-detection point-of-care test for use with clinician-collected vaginal samples. The test requires about 10 to 15 minutes for test results to become available; this test has a sensitivity of 82 to 95% and a specificity of 97 to 100%.[165,166] The Osom Trichomonas Rapid Test is not FDA-cleared for use in men.
- Solana Trichomonas Assay (Quidel): This point-of-care test uses isothermal Helicase-Dependent Amplification technology to detect T. vaginalis DNA from asymptomatic and symptomatic female urine specimens or clinician-collected vaginal specimens, with a sensitivity greater than 92% for urine specimens and greater than 98% for vaginal samples.[167] Results are available within 40 minutes. This test is not FDA-cleared for use in men.
- Sexual Health Click Test (Visby Medical): This point-of-care, CLIA-waived PCR test is a single-use, disposable test that can detect chlamydia, gonorrhea, and trichomonas using self-collected vaginal swabs.[168] The compact test device provides results within 30 minutes. In an analysis of self-collected vaginal swabs obtained in 1,449 women, this test had a sensitivity of 99.2% and specificity of 96.9% for detection of T. vaginalis.[168]
Screening Recommendations
Routine urogenital screening for trichomoniasis may be considered for (1) women receiving care in high trichomonas prevalence settings (STI clinics or correctional facilities), and 2) asymptomatic women at high risk of acquiring T. vaginalis (e.g., women with multiple sex partners, persons who exchange sex for money or drugs, or a history of STIs or incarceration).[147,169] Screening for trichomoniasis is recommended in all sexually active women with HIV (when they enter care and then annually thereafter).[147,169] Screening for T. vaginalis of the pharynx or rectum is not recommended, primarily because these infections are extremely uncommon, and the cost-effectiveness of screening at these sites has not been established.[147] Screening for trichomoniasis is not currently recommended for men.[169]
Treatment
Treatment of Trichomoniasis
All women diagnosed with trichomoniasis, regardless of HIV or pregnancy status, should receive treatment with metronidazole 500 mg twice daily for 7 days.[147] All men diagnosed with trichomoniasis, regardless of HIV status, should receive treatment with a single dose of 2 grams of oral metronidazole.[147] These recommendations are based on two studies conducted on women, most of whom were symptomatic, that demonstrated oral metronidazole given for 7 days was more effective at curing infection than a single 2-gram oral dose.[170,171] Tinidazole, given as a 2-gram oral dose, is the alternative for both women and men, but it should be avoided in pregnant women.[147] Experts now consider it unnecessary for persons to refrain from ingesting alcohol when they are taking metronidazole or tinidazole.[147] After the publication of the 2021 CDC STI guidelines, a single 2-gram oral dose of secnidazole, which has a longer half-life than both metronidazole and tinidazole, has been evaluated and FDA-approved for T. vaginalis treatment in females and males who are 12 years of age and older.[172,173,174] Metronidazole gel (intravaginal) is not effective for the treatment of trichomoniasis and is not recommended. Persons who are allergic to metronidazole should be referred to an allergy specialist; if this is not possible, additional options are limited but would include intravaginal paromomycin cream or intravaginal boric acid.[147,175,176,177]
Table 2. 2021 STI Treatment Guidelines: TrichomoniasisTreatment of TrichomoniasisRecommended Regimen for WomenMetronidazole500 mg orally twice a day for 7 daysMetronidazole
Tradename:FlagylRecommended Regimen for MenMetronidazole2 g orally in a single doseMetronidazole
Tradename:FlagylAlternative Regimen for Women and MenTinidazole2 g orally in a single doseTinidazole
Tradename:TindamaxSource: Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. Diseases characterized by vaginal itching, burning, irritation, odor or discharge: trichomoniasis. MMWR Recomm Rep. 2021;70(No. RR-4):1-187. [2021 STI Treatment Guidelines]Treatment of Persistent or Recurrent Trichomoniasis
The most likely reasons for persistent or recurrent trichomoniasis are reinfection from an untreated partner or lack of adherence with treatment, but in some individuals, antimicrobial-resistant T. vaginalis infection can occur. Rates of metronidazole resistance have ranged from 4 to 10%, and the rates of tinidazole resistance have been approximately 1%.[178,179] These resistance rate data are old and contemporary resistance data are needed, including resistance data with secnidazole. Tinidazole retains activity against many metronidazole-refractory strains. The following summarizes the approach to treatment in persons with persistent or recurrent trichomoniasis.[147]
- Treatment Failure with Reexposure: For women and men who received standard treatment for trichomoniasis and have treatment failure due to reexposure from an untreated partner, retreatment should consist of the same regimen they initially received.[147]
- Treatment Failure without Reexposure: For men who have treatment failure after receiving an initial single-dose therapy of metronidazole 2 grams orally (and reexposure has not occurred), the recommended retreatment is metronidazole 500 mg orally twice daily for 7 days.[147] For women who have failed the initial regimen of metronidazole 500 mg twice daily for 7 days and have not been reexposed, repeat treatment should be given with a 7-day regimen of either metronidazole 2 grams given once per day or tinidazole 2 grams once per day.[147] Tinidazole or secnidazole should not be used in pregnant women.
- Treatment Failure after Second-Line Treatment without Reexposure: If an individual experiences persistent infection after receiving treatment with a second-line regimen (and reexposure to a partner with trichomoniasis has not occurred), the clinician should request a special kit from the Centers for Disease Control and Prevention for 5-nitroimidazole drug-resistance testing (Trichomonas Susceptibility Testing).[147,180]
- Treatment of 5-Nitroimidazole-Resistant Trichomonas: If drug-resistance testing reveals nitroimidazole resistance and treatment with a 7-day regimen of either metronidazole 2 grams given once per day or tinidazole 2 grams once per day has been unsuccessful, then the next option is oral tinidazole 2 grams daily plus intravaginal tinidazole 500 mg twice daily for 14 days.[147,181] If this option fails, then consider using high-dose oral tinidazole (1 gram 3 times daily) plus intravaginal paromomycin (4 grams of 6.25% intravaginal paromomycin cream nightly) for 14 days.[147,177] A 14-day course of oral secnidazole 2 grams in combination with intravaginal boric acid 600 mg twice daily has also recently been used to successfully treat a case of persistent 5-nitroimidazole-resistant trichomoniasis.[182] Note that oral tinidazole or secnidazole should not be used in pregnant women. Intravaginal boric acid 600 mg twice daily for 60 days has been successfully used to treat trichomoniasis in women allergic to nitroimidazole and thus could be considered as an option for women with treatment-refractory nitroimidazole-resistant trichomoniasis.[147,176,183]
Management of Sex Partners
All persons diagnosed with trichomoniasis should refer all sex partners in the prior 60 days for evaluation, comprehensive STI testing, HIV testing, and presumptive treatment of trichomoniasis. All current sex partners should be referred for presumptive trichomoniasis therapy.[147] For persons diagnosed with trichomoniasis, expedited partner management (where a clinician provides presumptive antibiotic therapy and educational materials to a patient’s partner) may be considered in states where it is legally permitted (see the CDC United States Map for the Legal Status of Expedited Partner Therapy). Expedited partner management is permissible in most states.
Resumption of Sexual Activity
Persons diagnosed with trichomoniasis should be instructed to avoid sex until they and their sex partners have been treated and until they no longer have any symptoms of trichomoniasis. This usually takes about 7 days after completion of treatment.[147]
Post-Treatment Follow-Up
All sexually active women who are diagnosed and treated for T. vaginalis infection (including pregnant women and women with HIV) should be retested 3 months after initial treatment to evaluate the possibility of reinfection. Retesting in men is not routinely recommended.[147]
Treatment of Special Populations
- Treatment of Women During Pregnancy: Pregnant women with symptomatic trichomoniasis, in any trimester, should receive treatment with metronidazole 500 mg orally twice daily for 7 days.[147] Treatment of asymptomatic trichomoniasis in pregnancy, however, has not been shown to reduce preterm birth.[184] Both metronidazole and tinidazole are secreted in breast milk. Some clinicians advise deferring breastfeeding by 12-24 hours after taking a dose of metronidazole.[147,185] Tinidazole is not recommended during pregnancy due to limited animal studies suggesting fetal risk; women who are breastfeeding should wait 72 hours after taking tinidazole before breastfeeding.[147] Secnidazole is not currently recommended for use in pregnancy or during breastfeeding due to limited data.
- Treatment of Women with HIV: Women with HIV who are diagnosed with trichomoniasis should receive a 7-day treatment course of metronidazole 500 mg twice daily.[147,186] In women with HIV, the longer course of oral metronidazole therapy (500 mg twice daily for 7 days) has been shown to have higher cure rates than a 2 g single-dose of metronidazole (Figure 11).[141,186,187,188]
Patient Counseling and Education
Patient counseling and education should cover the nature of the disease, transmission issues, and risk reduction.
Nature of the Disease
- Trichomoniasis can be asymptomatic in men and women, and it may persist silently for years.
- Untreated trichomoniasis is associated with adverse pregnancy outcomes such as premature rupture of membranes, preterm delivery, and low birth weight infants.
- Infection with T. vaginalis in women has been associated with an increased risk of cervical cancer.
- Douching may worsen vaginal discharge in patients with trichomoniasis.
Transmission Issues
- Trichomoniasis is almost always sexually transmitted.
- Current and recent sex partners should undergo evaluation and receive empiric treatment for trichomoniasis.
- Persons diagnosed with trichomoniasis should abstain from intercourse until they and their sex partners are cured (about 7 days).
- Trichomoniasis has been associated with increased susceptibility to HIV acquisition and transmission.
Risk Reduction
- Individualize risk-reduction plans with each patient.
- Prevention strategies include abstinence, mutual monogamy with an uninfected partner, consistent condom use, and limiting the number of sex partners.
- Douching should be avoided since it increases the risk for trichomoniasis.
- Male circumcision reduces the risk of trichomoniasis.[189,190]
Vulvovaginal Candidiasis
Introduction
Vulvovaginal candidiasis is caused by an abnormal proliferation of one or more Candida species in the vaginal tract. Vulvovaginal candidiasis is commonly referred to as a “yeast” infection. Globally, about 138 million women have vulvovaginal candidiasis on an annual basis.[191,192] Although vulvovaginal candidiasis is not a sexually transmitted infection, it frequently causes clinical manifestations that overlap with other sexually transmitted infections and vaginal conditions.
Epidemiology
An estimated 70 to 75% of women will experience at least one episode of vulvovaginal candidiasis in their lifetime, 40 to 50% will experience a second episode, and approximately 5 to 10% will develop recurrent vulvovaginal candidiasis (defined as three or more symptomatic episodes in one year).[192,193,194] Overall, candidiasis is responsible for about 15 to 30% of all cases of vaginitis.[195] Candidiasis is the second most common cause of vaginal infections after bacterial vaginosis, though information on the incidence of vulvovaginal candidiasis is incomplete since vulvovaginal candidiasis is not reportable.[196] Women with HIV have more frequent episodes of vulvovaginal candidiasis than women without HIV.[197,198] In addition, with more advanced HIV disease, vulvovaginal candidiasis is often more severe and may recur more frequently.
Pathogenesis and Microbiology
Candida species are normal flora of the vagina and are not considered a sexually transmitted pathogen. Indeed, an estimated 20% of healthy women who have no vulvovaginal symptoms will have Candida species isolated from their vagina.[192] Disruption in the host vaginal environment, however, can cause Candida organisms to transition from a commensal to a pathogenic role.[193] Yeast blastospores are typically responsible for asymptomatic colonization, whereas mycelia (pseudohyphae or hyphae forms) cause symptomatic vaginitis through overgrowth and adherence to vaginal epithelial cells (Figure 12).[192] Destruction of host tissue by Candida species is mediated by hydrolytic enzymes that promote adhesion and host tissue penetration, as well as other virulence factors, such as biofilm formation and phenotypic switching.[193] In the United States, Candida albicans strains are responsible for 85 to 95% of cases of vulvovaginal candidiasis, with the remainder due to non-albicans Candida isolates, most commonly C. glabrata.[192] Fluconazole resistance is most often associated with significant prior azole exposure.[199,200]
Factors Associated with Vulvovaginal Candidiasis
Although most women with vulvovaginal candidiasis do not have specific risk factors associated with vulvovaginal candidiasis, those with frequent, complicated, and/or severe vulvovaginal candidiasis have a number of factors that have been identified, including host factors (uncontrolled diabetes, corticosteroids, repeated courses of antibiotics, pregnancy, HIV, hormone replacement therapy), behavioral factors (sexual practices, use of oral contraceptives, intrauterine devices, condoms, and spermicide), and genetic predisposition.[192,193,194]
Classification of Vulvovaginal Candidiasis
On the basis of clinical presentation, host immunity, and pathogen factors, vulvovaginal candidiasis is classified as either uncomplicated or complicated (Table 3).[198,201,202] Among all women who develop vulvovaginal candidiasis, approximately 10 to 20% will have complicated vulvovaginal candidiasis. Distinguishing uncomplicated from complicated vulvovaginal candidiasis is important, as it influences treatment decisions in most instances. The management of complicated vulvovaginal candidiasis requires unique diagnostic and treatment considerations.[198]
Clinical Manifestations
Vulvovaginal candidiasis characteristically manifests with multiple vaginal symptoms that may include pruritus, vaginal soreness, dyspareunia, external vulvar burning, external dysuria, and, in some, abnormal vaginal discharge.[2,192,195] When vaginal discharge is present, it is typically described as odorless, thick, white, and clumpy (“cottage-cheese-like”) (Figure 13), but it may be thin or watery.[192] Vulvar and labial erythema, fissures, and satellite papular lesions may also be present.[192] Symptoms associated with vulvovaginal candidiasis tend to flare prior to the onset of menses.
Diagnostic Methods
The clinical symptoms of vulvovaginal candidiasis overlap with other causes of vaginitis, so diagnostic evaluation is recommended. Most women with symptomatic vulvovaginal candidiasis can be readily diagnosed based on a microscopic examination of vaginal secretions. A vaginal Gram stain is not recommended for the diagnosis of vulvovaginal candidiasis.
- Vaginal pH: The vaginal pH is typically normal (less than 4.5) in the setting of vulvovaginal candidiasis. If the pH is abnormally high (greater than 4.5), it suggests an alternative diagnosis of bacterial vaginosis, trichomoniasis, or a mixed vaginal infection.
- Wet Mount with Potassium Hydroxide (KOH) and/or Saline: Visualization under microscopy of pseudohyphae (mycelia) and/or budding yeast (conidia) on 10% KOH wet prep examination or saline wet mount can confirm the diagnosis of candidiasis (Figure 14). Use of the 10% KOH preparation dissolves many of the host cells and thus improves sensitivity when compared with the saline wet mount.[192] Microscopy is also useful in differentiating candidiasis from bacterial vaginosis and T. vaginalis. Most women with vulvovaginal candidiasis do not have abundant white blood cells visualized on microscopy. Large numbers of white blood cells indicate a mixed infection or a diagnosis other than vulvovaginal candidiasis.
- Culture: For those with negative wet mounts but existing signs or symptoms worrisome for vulvovaginal candidiasis, fungal culture for Candida species should be considered. Identifying Candida species by vaginal fungal culture in the absence of symptoms or signs is not an indication for treatment because approximately 10 to 20% of healthy women harbor Candida species in the vagina.[192] In women with complicated vulvovaginal candidiasis, however, fungal cultures are indicated to confirm the diagnosis and to detect non-albicans species; this is particularly important for identifying C. glabrata since this organism only forms blastospores and is easily missed on microscopy.[198] In addition, fungal cultures (with resistance testing) should be performed in women with recurrent vulvovaginal candidiasis who have persistent symptoms while receiving maintenance antifungal therapy.[198,200] Because non-albicans species are present in about 10 to 20% of women with recurrent vulvovaginal candidiasis, some experts would obtain vaginal fungal cultures prior to initiating suppressive therapy for vulvovaginal candidiasis.
- Nucleic Acid Amplification Tests: There are now multiple FDA-approved NAAT tests for diagnosing vulvovaginal candidiasis in symptomatic women.
- BD Max Vaginal Panel (Beckton Dickinson): Candida results reported from the BD Max Vaginal Panel include Candida species group (C. albicans, C. tropicalis, C. parapsilosis, C. dubliniensis) and C. glabrata-C. krusei. Test sensitivity is 90.9%, and specificity is 94.1% for the Candida species group. Sensitivity for C. glabrata was 75.9%, and specificity was 99.7%.
- Aptima CV/TV Assay (Hologic): Candida results reported from this assay include Candida species group (C. albicans, C. tropicalis, C. parapsilosis, C. dubliniensis) and C. glabrata. The sensitivity and specificity of this assay are 91.7% and 94.9% for the Candida species group and 84.7% and 99.1% for C. glabrata, respectively.
- Gene Xpert Xpress MVP (Cepheid): The Xpert Xpress MVP is a CLIA-waived on-demand diagnostic PCR test that detects DNA targets Candida species as well as T. aginalis and anaerobic bacteria associated with BV (F. vaginae, BVAB-2, and Megasphaera type 1). Results related to Candida report Candida spp. group (C. albicans, C. tropicalis, C. parapsilosis, C. dubliniensis) and C. glabrata-C. krusei.
Treatment of Uncomplicated Vulvovaginal Candidiasis
Treatment Options
There are multiple recommended short-course, over-the-counter, and prescription formulations for intravaginal antifungal treatments for women with uncomplicated vulvovaginal candidiasis.[198] For women who prefer oral therapy, 150 mg of fluconazole in a single dose is an option.[198] In addition, ibrexafungerp, a novel oral glucan synthase inhibitor, was FDA-approved in June 2021 for the treatment of uncomplicated candidal vulvovaginitis; ibrexafungerp is dosed 300 mg orally twice daily for one day (this medication is not currently available in the United States due to problems with production).[203,204] The short-course topical formulations are effective in treating uncomplicated vulvovaginal candidiasis, and topical azole drugs are more effective than topical nystatin. An estimated 80 to 90% of women with vulvovaginal candidiasis who complete treatment with an azole have relief in symptoms and negative fungal cultures. Of note, the topical intravaginal azole creams and suppositories are oil-based and may potentially weaken latex condoms and diaphragms.[198] Thus, women receiving treatment with a topical antifungal intravaginal cream should abstain from sex during treatment or use a form of birth control that does not rely on a condom or diaphragm.
Table 4. 2021 STI Treatment Guidelines: Vulvovaginal CandidiasisTreatment of Uncomplicated Vulvovaginal CandidiasisRecommended Regimens: Over-the-Counter Intravaginal AgentsClotrimazole 1% cream5 g intravaginally daily for 7–14 daysClotrimazole 1% cream
Tradename:Recommended Regimens: Over-the-Counter Intravaginal AgentsClotrimazole 2% cream5 g intravaginally daily for 3 daysClotrimazole 2% cream
Tradename:Recommended Regimens: Over-the-Counter Intravaginal AgentsMiconazole 2% cream5 g intravaginally daily for 7 daysMiconazole 2% cream
Tradename:MonistatRecommended Regimens: Over-the-Counter Intravaginal AgentsMiconazole 4% cream5 g intravaginally daily for 3 daysMiconazole 4% cream
Tradename:Recommended Regimens: Over-the-Counter Intravaginal AgentsMiconazole 100 mg vaginal supositoryone suppository daily for 7 daysMiconazole 100 mg vaginal supository
Tradename:Monistat 7Recommended Regimens: Over-the-Counter Intravaginal AgentsMiconazole 200 mg vaginal suppositoryone suppository daily for 3 daysMiconazole 200 mg vaginal suppository
Tradename:Monistat 3Recommended Regimens: Over-the-Counter Intravaginal AgentsMiconazole 1,200 mg vaginal suppositoryone suppository for 1 dayMiconazole 1,200 mg vaginal suppository
Tradename:Monistat 1Recommended Regimens: Over-the-Counter Intravaginal AgentsTioconazole 6.5% ointment5 g intravaginally in a single applicationTioconazole 6.5% ointment
Tradename:Vagistat-1Recommended Regimens: Prescription Intravaginal AgentsButoconazole 2% cream (single dose bioadhesive product)5 g intravaginally in a single applicationButoconazole 2% cream (single dose bioadhesive product)
Tradename:GynazoleRecommended Regimens: Prescription Intravaginal AgentsTerconazole 0.4% cream5 g intravaginally daily for 7 daysTerconazole 0.4% cream
Tradename:Terazol 7Recommended Regimens: Prescription Intravaginal AgentsTerconazole 0.8% cream5 g intravaginally daily for 3 daysTerconazole 0.8% cream
Tradename:Terazol 3Recommended Regimens: Prescription Intravaginal AgentsTerconazole 80 mg vaginal suppositoryone suppository daily for 3 daysTerconazole 80 mg vaginal suppository
Tradename:Terazol 3 SuppositoryRecommended Regimen: Oral AgentFluconazole150 mg orally in a single doseFluconazole
Tradename:DiflucanNote: the creams and suppositories in these regimens are oil based and might weaken latex condoms and diaphragms. Patients should refer to condom product labeling for further information.Source: Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. Diseases characterized by vaginal itching, burning, irritation, odor or discharge: vulvovaginal candidiasis. MMWR Recomm Rep. 2021;70(No. RR-4):1-187. [2021 STI Treatment Guidelines]Management of Sex Partners
Since vulvovaginal candidiasis is not sexually transmitted, there is no treatment necessary for asymptomatic sex partners of women with uncomplicated vulvovaginal candidiasis. Balanitis caused by Candida species is an uncommon finding in men and may be due to factors other than penile-vaginal sex, including age over 40, diabetes mellitus, or uncircumcised status.[205] Men with Candida balanitis should be treated with 7 days of topical antifungal therapy, or a single 150-mg dose of oral fluconazole.[205,206]
Post-Treatment Follow-Up
Follow-up after treatment of uncomplicated vulvovaginal candidiasis is not necessary. Women should seek reevaluation if symptoms persist or recur, since this could indicate complicated disease.
Treatment of Complicated Vulvovaginal Candidiasis
Treatment of Severe Vulvovaginal Candidiasis
Severe disease, which can involve significant skin breakdown, fissuring, and edema, requires treatment with 7 to 14 days of topical azole therapy or two doses of oral fluconazole 150 mg given 72 hours apart.[198]
Treatment of Recurrent Vulvovaginal Candidiasis
Recurrent vulvovaginal candidiasis—defined as three or more episodes within one year—occurs in fewer than 5% of women with vulvovaginal candidiasis.[191] Among women with recurrent disease, approximately 10 to 20% will have non-albicans species, including C. glabrata, isolated from vaginal cultures. Although most women with recurrent vulvovaginal candidiasis have no predisposing or underlying conditions, some will have a risk factor, such as frequent antibiotic use, diabetes mellitus, or immunosuppression. If culture results show C. albicans, the recommended approach is to use a longer 7- to 14-day initial course of therapy to achieve clinical remission, followed by a 6-month maintenance regimen.[198] The goal of the intensive initial therapy is to achieve mycologic remission before initiating maintenance therapy.
- Fluconazole: The preferred oral initial therapy consists of fluconazole given as a 100 mg, 150 mg, or 200 mg oral dose every third day (days 1, 4, and 7) for a total of 3 doses. The preferred maintenance therapy consists of oral fluconazole (100, 150, or 200 mg) given weekly for 6 months; maintenance therapy has been demonstrated to reduce episodes of vulvovaginal candidiasis, but symptoms recur in about 30 to 50% of women once maintenance therapy is stopped.
- Topical Intravaginal Imidazole Therapy: The use of topical therapy for 7 to 14 days is an option for the initial course. Typically, this is followed by oral fluconazole maintenance therapy. For women who cannot take oral fluconazole maintenance therapy, topical azole therapy given intermittently can be used as an alternative.
- Oteseconazole: In 2022, oral oteseconazole was FDA-approved for the treatment of recurrent candidiasis in women who are not of reproductive potential. This approval occurred following several randomized, controlled trials that showed high efficacy of oteseconazole in reducing the incidence of recurrent vulvovaginal infections.[207,208] The recommended dosing for oral oteseconazole is 600 mg orally on day 1, then 450 mg on day 2, then beginning on day 14, weekly 150 mg oral dosing for 11 weeks. Alternatively, oteseconazole can be started following an initial course of oral fluconazole. With this approach, oral fluconazole is given as a 150 mg dose every 72 hours for three doses (given on days 1, 4, and 7), and then on days 14-20, oteseconazole is given as 150-mg oral daily dosing for 6 days, followed by weekly 150 mg dosing beginning on day 28 and continued for 11 weeks.
- Ibrexafungerp: In 2022, ibrexafungerp was FDA-approved for the treatment of recurrent candidiasis. Ibrexafungerp is dosed orally 300 mg twice daily for six months following administration of fluconazole 150 mg orally every 72 hours for three doses.[209] This medication was recalled in September 2023 due to possible cross-contamination with a non-antibacterial drug, and it has not been available since the recall.
Treatment of Non-albicans Vulvovaginal Candidiasis
There are limited data on the treatment of non-albicans vulvovaginal candidiasis, and the optimal treatment approach is not known.[210] Strategies usually employ treatment of non-albicans vulvovaginal candidiasis with a 7- to 14-day course of a non-fluconazole azole, either oral or topical.[198] If this approach fails, intravaginal boric acid (600 mg in a gelatin capsule inserted nightly for 3 weeks) is a reasonable option, with expected high clinical and mycologic response rates.[198,210,211] If all of these measures fail, consultation with a specialist is advised.
Treatment of Immunocompromised Women
Women with diabetes, underlying immunodeficiency, or immunosuppressive therapy (e.g. chronic corticosteroids) should receive longer courses of antifungal therapy—typically a course lasting 7 to 14 days.[198]
Treatment of Women with HIV
Women with HIV and vulvovaginal candidiasis (complicated or uncomplicated) should receive the same treatment as women without HIV.[198] If topical therapies are chosen, it is especially important to counsel women with HIV that the available creams and suppositories are oil-based and might weaken latex condoms. With more advanced HIV disease, vulvovaginal candidiasis is often more severe and may recur more frequently, but primary prophylactic fluconazole therapy is not recommended in these women.[198,212]Treatment of Women During Pregnancy
The recommended treatment of vulvovaginal candidiasis in pregnant women is a 7-day course of a topical (intravaginal) azole cream.[198] Oral fluconazole should not be used in pregnancy due to several reports that suggested a possible association of oral fluconazole with spontaneous abortion and possible teratogenicity.[213,214] Both oteseconazole and ibrexafungerp are contraindicated for use during pregnancy.[215]
Management of Sex Partners
Insufficient data exist regarding the treatment of sex partners of women who have complicated vulvovaginal candidiasis. Accordingly, there are no recommendations for or against treating male sex partners in this setting.[198]
Counseling and Education
Patient counseling and education about vulvovaginal candidiasis should cover the nature of the disease, transmission issues, and risk reduction.
Nature of the Disease
- Asymptomatic colonization with Candida species is common and does not require treatment.
- Symptomatic vulvovaginal candidiasis is caused by a disruption of the normal vaginal microbiota by various factors, including pregnancy, diabetes, hormonal contraception, sexual activity, and immunosuppressive conditions.
- Women with symptomatic vulvovaginal candidiasis should be treated with antifungal therapy.
- Women with complicated vulvovaginal candidiasis typically require longer courses of antifungal therapy.
Transmission Issues
- Vulvovaginal candidiasis is not considered a sexually transmitted infection, although there are some cases of male sex partners developing Candida balanitis as a result of penile-vaginal sex.
Risk Reduction
- Avoid douching.
- Avoid unnecessary antibiotic use.
- Avoid repeated courses of self-administered, over-the-counter antifungal therapy in settings where no laboratory diagnosis has been confirmed.
- Complete the full course of any prescribed therapy.
- Optimize the management of other concurrent illnesses, such as diabetes mellitus and HIV.
Summary Points
- The three most common conditions diagnosed among women with vaginal symptoms presenting in the primary care setting are bacterial vaginosis, vulvovaginal candidiasis, and trichomoniasis.
- The normal vagina has abundant and dominant Lactobacillus species and a pH that is less than 3.8 to 4.5.
- Vaginitis is primarily a clinical diagnosis, but a wide variety of diagnostic tests are available, including point-of-care tests, culture, molecular detection methods (PCR, NAAT), and indirect testing for enzymatic activity.
- Women with symptomatic bacterial vaginosis typically present with a homogenous, white or gray vaginal discharge that often has a “fishy” odor. Bacterial vaginosis has been linked to several obstetrical and gynecologic complications.
- The preferred treatments for bacterial vaginosis are oral metronidazole (500 mg twice daily for 7 days), 0.75% metronidazole gel (5 grams applied intravaginally once daily for 5 days), or intravaginal 2% clindamycin cream (5 grams applied intravaginally at bedtime for 7 days).
- Women with symptomatic trichomoniasis usually have a characteristic “frothy” gray or yellow-green vaginal discharge and pruritus. Trichomoniasis increases the risk of premature rupture of membranes and preterm labor.
- The preferred treatment for trichomoniasis in women is a 7-day course of oral metronidazole (500 mg twice daily); for men, the preferred treatment is a single 2-gram dose of oral metronidazole.
- Vulvovaginal candidiasis characteristically presents with symptoms of pruritus, vaginal soreness, dyspareunia, vulvar burning, external dysuria, and abnormal vaginal discharge.
- Vulvovaginal candidiasis is classified as either uncomplicated or complicated based on clinical presentation, host immunity, and pathogen factors.
- Uncomplicated vulvovaginal candidiasis can be treated with a wide array of short-course topical antifungal agents or a single 150 mg dose of oral fluconazole.
Check-On-Learning Questions Display Options
These quick questions are meant to keep you on track and check your understanding. They appear throughout the core concepts and are listed here for you to review.Citations
- 1.Yarbrough ML, Burnham CA. The ABCs of STIs: An Update on sexually transmitted infections. Clin Chem. 2016;62:811-23.[PubMed Abstract] -
- 2.Anderson MR, Klink K, Cohrssen A. Evaluation of vaginal complaints. JAMA. 2004;291:1368-79.[PubMed Abstract] -
- 3.Hainer BL, Gibson MV. Vaginitis. Am Fam Physician. 2011;83:807-15.[PubMed Abstract] -
- 4.Rivers CA, Adaramola OO, Schwebke JR. Prevalence of bacterial vaginosis and vulvovaginal candidiasis mixed infection in a southeastern american STD clinic. Sex Transm Dis. 2011;38:672-4.[PubMed Abstract] -
- 5.Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. Diseases characterized by vaginal itching, burning, irritation, odor or discharge. MMWR Recomm Rep. 2021;70(No. RR-4):1-187.
- 6.Egan ME, Lipsky MS. Diagnosis of vaginitis. Am Fam Physician. 2000;62:1095-104.[PubMed Abstract] -
- 7.Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29:297-301.[PubMed Abstract] -
- 8.Haefner HK. Current evaluation and management of vulvovaginitis. Clin Obstet Gynecol. 1999;42:184-95.[PubMed Abstract] -
- 9.Bachmann LH, Hobbs MM, Seña AC, et al. Trichomonas vaginalis genital infections: progress and challenges. Clin Infect Dis. 2011;53 Suppl 3:S160-72.[PubMed Abstract] -
- 10.Hobbs MM, Seña AC. Modern diagnosis of Trichomonas vaginalis infection. Sex Transm Infect. 2013;89:434-8.[PubMed Abstract] -
- 11.Schwebke JR, Taylor SN, Ackerman R, et al. Clinical Validation of the Aptima Bacterial Vaginosis and Aptima Candida/Trichomonas Vaginitis Assays: Results from a Prospective Multicenter Clinical Study. J Clin Microbiol. 2020;58:e01643-19.[PubMed Abstract] -
- 12.Coleman JS, Gaydos CA. Molecular diagnosis of bacterial vaginosis: an update. J Clin Microbiol. 2018;56:e00342-18.[PubMed Abstract] -
- 13.Van Gerwen OT, Muzny CA. Recent advances in the epidemiology, diagnosis, and management of Trichomonas vaginalis infection. F1000Res. 2019;8:F1000 Faculty Rev-1666.[PubMed Abstract] -
- 14.Muzny CA, Łaniewski P, Schwebke JR, Herbst-Kralovetz MM. Host-vaginal microbiota interactions in the pathogenesis of bacterial vaginosis. Curr Opin Infect Dis. 2020;33:59-65.[PubMed Abstract] -
- 15.Fredricks DN, Fiedler TL, Marrazzo JM. Molecular identification of bacteria associated with bacterial vaginosis. N Engl J Med. 2005;353:1899-911.[PubMed Abstract] -
- 16.Muzny CA, Taylor CM, Swords WE, et al. An updated conceptual model on the pathogenesis of bacterial vaginosis. J Infect Dis. 2019;220:1399-1405.[PubMed Abstract] -
- 17.Hillier SL, Nugent RP, Eschenbach DA, et al. Association between bacterial vaginosis and preterm delivery of a low-birth-weight infant. The Vaginal Infections and Prematurity Study Group. N Engl J Med. 1995;333:1737-42.[PubMed Abstract] -
- 18.Koumans EH, Sternberg M, Bruce C, et al. The prevalence of bacterial vaginosis in the United States, 2001-2004; associations with symptoms, sexual behaviors, and reproductive health. Sex Transm Dis. 2007;34:864-9.[PubMed Abstract] -
- 19.Allsworth JE, Peipert JF. Prevalence of bacterial vaginosis: 2001-2004 National Health and Nutrition Examination Survey data. Obstet Gynecol. 2007;109:114-20.[PubMed Abstract] -
- 20.Peebles K, Velloza J, Balkus JE, McClelland RS, Barnabas RV. High global burden and costs of bacterial vaginosis: a systematic review and meta-analysis. Sex Transm Dis. 2019;46:304-11.[PubMed Abstract] -
- 21.Bautista CT, Wurapa E, Sateren WB, Morris S, Hollingsworth B, Sanchez JL. Bacterial vaginosis: a synthesis of the literature on etiology, prevalence, risk factors, and relationship with chlamydia and gonorrhea infections. Mil Med Res. 2016;3:4.[PubMed Abstract] -
- 22.Klebanoff MA, Nansel TR, Brotman RM, et al. Personal hygienic behaviors and bacterial vaginosis. Sex Transm Dis. 2010;37:94-9.[PubMed Abstract] -
- 23.Klebanoff MA, Andrews WW, Zhang J, et al. Race of male sex partners and occurrence of bacterial vaginosis. Sex Transm Dis. 2010;37:184-90.[PubMed Abstract] -
- 24.Marrazzo JM, Thomas KK, Fiedler TL, Ringwood K, Fredricks DN. Relationship of specific vaginal bacteria and bacterial vaginosis treatment failure in women who have sex with women. Ann Intern Med. 2008;149:20-8.[PubMed Abstract] -
- 25.Schwebke JR, Desmond R. Risk factors for bacterial vaginosis in women at high risk for sexually transmitted diseases. Sex Transm Dis. 2005;32:654-8.[PubMed Abstract] -
- 26.Bradshaw CS, Vodstrcil LA, Hocking JS, et al. Recurrence of bacterial vaginosis is significantly associated with posttreatment sexual activities and hormonal contraceptive use. Clin Infect Dis. 2013;56:777-86.[PubMed Abstract] -
- 27.Marrazzo JM, Thomas KK, Fiedler TL, Ringwood K, Fredricks DN. Risks for acquisition of bacterial vaginosis among women who report sex with women: a cohort study. PLoS One. 2010;5:e11139.[PubMed Abstract] -
- 28.Bradshaw CS, Sobel JD. Current Treatment of bacterial vaginosis-limitations and need for innovation. J Infect Dis. 2016;214 Suppl 1:S14-20.[PubMed Abstract] -
- 29.Brotman RM, Erbelding EJ, Jamshidi RM, Klebanoff MA, Zenilman JM, Ghanem KG. Findings associated with recurrence of bacterial vaginosis among adolescents attending sexually transmitted diseases clinics. J Pediatr Adolesc Gynecol. 2007;20:225-31.[PubMed Abstract] -
- 30.Marrazzo JM, Koutsky LA, Eschenbach DA, Agnew K, Stine K, Hillier SL. Characterization of vaginal flora and bacterial vaginosis in women who have sex with women. J Infect Dis. 2002;185:1307-13.[PubMed Abstract] -
- 31.Mitchell C, Manhart LE, Thomas KK, Agnew K, Marrazzo JM. Effect of sexual activity on vaginal colonization with hydrogen peroxide-producing lactobacilli and Gardnerella vaginalis. Sex Transm Dis. 2011;38:1137-44.[PubMed Abstract] -
- 32.Vodstrcil LA, Plummer EL, Fairley CK, et al. Male-Partner Treatment to Prevent Recurrence of Bacterial Vaginosis. N Engl J Med. 2025;392:947-57.[PubMed Abstract] -
- 33.Muzny CA, Sobel JD. Bacterial Vaginosis - Time to Treat Male Partners. N Engl J Med. 2025;392:1026-7.[PubMed Abstract] -
- 34.Berger BJ, Kolton S, Zenilman JM, Cummings MC, Feldman J, McCormack WM. Bacterial vaginosis in lesbians: a sexually transmitted disease. Clin Infect Dis. 1995;21:1402-5.[PubMed Abstract] -
- 35.Fethers KA, Fairley CK, Morton A, et al. Early sexual experiences and risk factors for bacterial vaginosis. J Infect Dis. 2009;200:1662-70.[PubMed Abstract] -
- 36.Liu CM, Hungate BA, Tobian AA, et al. Penile microbiota and female partner bacterial vaginosis in Rakai, Uganda. MBio. 2015;6:e00589.[PubMed Abstract] -
- 37.Vodstrcil LA, Walker SM, Hocking JS, et al. Incident bacterial vaginosis (BV) in women who have sex with women is associated with behaviors that suggest sexual transmission of BV. Clin Infect Dis. 2015;60:1042-53.[PubMed Abstract] -
- 38.Mitchell C, Marrazzo J. Bacterial vaginosis and the cervicovaginal immune response. Am J Reprod Immunol. 2014;71:555-63.[PubMed Abstract] -
- 39.Muzny CA, Blanchard E, Taylor CM, et al. Identification of key bacteria involved in the induction of incident bacterial vaginosis: a prospective study. J Infect Dis. 2018;218:966-78.[PubMed Abstract] -
- 40.Sousa M, Ksiezarek M, Perovic SU, et al. Gardnerella pickettii sp. nov. (formerly Gardnerella genomic species 3) and Gardnerella greenwoodii sp. nov. (formerly Gardnerella genomic species 8) isolated from female urinary microbiome. Int J Syst Evol Microbiol. 2023;73(11).[PubMed Abstract] -
- 41.Vaneechoutte M, Guschin A, Van Simaey L, Gansemans Y, Van Nieuwerburgh F, Cools P. Emended description of Gardnerella vaginalis and description of Gardnerella leopoldii sp. nov., Gardnerella piotii sp. nov. and Gardnerella swidsinskii sp. nov., with delineation of 13 genomic species within the genus Gardnerella. Int J Syst Evol Microbiol. 2019;69:679-87.[PubMed Abstract] -
- 42.Klebanoff MA, Schwebke JR, Zhang J, Nansel TR, Yu KF, Andrews WW. Vulvovaginal symptoms in women with bacterial vaginosis. Obstet Gynecol. 2004;104:267-72.[PubMed Abstract] -
- 43.Eschenbach DA, Hillier S, Critchlow C, Stevens C, DeRouen T, Holmes KK. Diagnosis and clinical manifestations of bacterial vaginosis. Am J Obstet Gynecol. 1988;158:819-28.[PubMed Abstract] -
- 44.Reiter S, Kellogg Spadt S. Bacterial vaginosis: a primer for clinicians. Postgrad Med. 2019;131:8-18.[PubMed Abstract] -
- 45.Bilardi JE, Walker S, Temple-Smith M, et al. The burden of bacterial vaginosis: women's experience of the physical, emotional, sexual and social impact of living with recurrent bacterial vaginosis. PLoS One. 2013;8:e74378.[PubMed Abstract] -
- 46.Berger A, Kane KY. Clindamycin for vaginosis reduces prematurity and late miscarriage. J Fam Pract. 2003;52:603-4.[PubMed Abstract] -
- 47.Laxmi U, Agrawal S, Raghunandan C, Randhawa VS, Saili A. Association of bacterial vaginosis with adverse fetomaternal outcome in women with spontaneous preterm labor: a prospective cohort study. J Matern Fetal Neonatal Med. 2012;25:64-7.[PubMed Abstract] -
- 48.Nelson DB, Hanlon A, Hassan S, et al. Preterm labor and bacterial vaginosis-associated bacteria among urban women. J Perinat Med. 2009;37:130-4.[PubMed Abstract] -
- 49.Oakeshott P, Kerry S, Hay S, Hay P. Bacterial vaginosis and preterm birth: a prospective community-based cohort study. Br J Gen Pract. 2004;54:119-22.[PubMed Abstract] -
- 50.Soper DE. Bacterial vaginosis and postoperative infections. Am J Obstet Gynecol. 1993;169:467-9.[PubMed Abstract] -
- 51.Ravel J, Moreno I, Simón C. Bacterial vaginosis and its association with infertility, endometritis, and pelvic inflammatory disease. Am J Obstet Gynecol. 2021;224:251-7.[PubMed Abstract] -
- 52.Cherpes TL, Wiesenfeld HC, Melan MA, et al. The associations between pelvic inflammatory disease, Trichomonas vaginalis infection, and positive herpes simplex virus type 2 serology. Sex Transm Dis. 2006;33:747-52.[PubMed Abstract] -
- 53.Lokken EM, Balkus JE, Kiarie J, et al. Association of Recent Bacterial Vaginosis With Acquisition of Mycoplasma genitalium. Am J Epidemiol. 2017;186:194-201.[PubMed Abstract] -
- 54.Brotman RM, Klebanoff MA, Nansel TR, et al. Bacterial vaginosis assessed by gram stain and diminished colonization resistance to incident gonococcal, chlamydial, and trichomonal genital infection. J Infect Dis. 2010;202:1907-15.[PubMed Abstract] -
- 55.Cherpes TL, Meyn LA, Krohn MA, Lurie JG, Hillier SL. Association between acquisition of herpes simplex virus type 2 in women and bacterial vaginosis. Clin Infect Dis. 2003;37:319-25.[PubMed Abstract] -
- 56.Martin HL, Richardson BA, Nyange PM, et al. Vaginal lactobacilli, microbial flora, and risk of human immunodeficiency virus type 1 and sexually transmitted disease acquisition. J Infect Dis. 1999;180:1863-8.[PubMed Abstract] -
- 57.Abbai NS, Reddy T, Ramjee G. Prevalent bacterial vaginosis infection - a risk factor for incident sexually transmitted infections in women in Durban, South Africa. Int J STD AIDS. 2016;27:1283-8.[PubMed Abstract] -
- 58.Brusselaers N, Shrestha S, van de Wijgert J, Verstraelen H. Vaginal dysbiosis and the risk of human papillomavirus and cervical cancer: systematic review and meta-analysis. Am J Obstet Gynecol. 2019221:9-18.e8.[PubMed Abstract] -
- 59.McClelland RS, Lingappa JR, Srinivasan S, et al. Evaluation of the association between the concentrations of key vaginal bacteria and the increased risk of HIV acquisition in African women from five cohorts: a nested case-control study. Lancet Infect Dis. 2018;18:554-64.[PubMed Abstract] -
- 60.Passmore JS, Jaspan HB. Vaginal microbes, inflammation, and HIV risk in African women. Lancet Infect Dis. 2018;18:483-4.[PubMed Abstract] -
- 61.Cohen CR, Lingappa JR, Baeten JM, et al. Bacterial vaginosis associated with increased risk of female-to-male HIV-1 transmission: a prospective cohort analysis among African couples. PLoS Med. 2012;9:e1001251.[PubMed Abstract] -
- 62.Muzny CA, Cerca N, Elnaggar JH, Taylor CM, Sobel JD, Van Der Pol B. State of the Art for Diagnosis of Bacterial Vaginosis. J Clin Microbiol. 2023;61:e0083722.[PubMed Abstract] -
- 63.Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. Diseases characterized by vaginal itching, burning, irritation, odor or discharge: bacterial vaginosis. MMWR Recomm Rep. 2021;70(No. RR-4):1-187.
- 64.Karani A, De Vuyst H, Luchters S, et al. The Pap smear for detection of bacterial vaginosis. Int J Gynaecol Obstet. 2007;98:20-3.[PubMed Abstract] -
- 65.Tokyol C, Aktepe OC, Cevrioğlu AS, Altindiş M, Dilek FH. Bacterial vaginosis: comparison of Pap smear and microbiological test results. Mod Pathol. 2004;17:857-60.[PubMed Abstract] -
- 66.Heller DS, Pitsos M, Skurnick J. Does the presence of vaginitis on a Pap smear correlate with clinical symptoms in the patient? J Reprod Med. 2008;53:429-34.[PubMed Abstract] -
- 67.Amsel R, Totten PA, Spiegel CA, Chen KC, Eschenbach D, Holmes KK. Nonspecific vaginitis. Diagnostic criteria and microbial and epidemiologic associations. Am J Med. 1983;74:14-22.[PubMed Abstract] -
- 68.Mills BB. Vaginitis: Beyond the Basics. Obstet Gynecol Clin North Am. 2017;44:159-177.[PubMed Abstract] -
- 69.Bradshaw CS, Morton AN, Garland SM, Horvath LB, Kuzevska I, Fairley CK. Evaluation of a point-of-care test, BVBlue, and clinical and laboratory criteria for diagnosis of bacterial vaginosis. J Clin Microbiol. 2005;43:1304-8.[PubMed Abstract] -
- 70.Myziuk L, Romanowski B, Johnson SC. BVBlue test for diagnosis of bacterial vaginosis. J Clin Microbiol. 2003;41:1925-8.[PubMed Abstract] -
- 71.West B, Morison L, Schim van der Loeff M, et al. Evaluation of a new rapid diagnostic kit (FemExam) for bacterial vaginosis in patients with vaginal discharge syndrome in The Gambia. Sex Transm Dis. 2003;30:483-9.[PubMed Abstract] -
- 72.Gaydos CA, Beqaj S, Schwebke JR, et al. Clinical validation of a test for the diagnosis of vaginitis. Obstet Gynecol. 2017;130:181-9.[PubMed Abstract] -
- 73.Schwebke JR, Taylor SN, Ackerman R, et al. Clinical validation of the Aptima bacterial vaginosis and Aptima Candida/Trichomonas vaginitis assays: results from a prospective multicenter clinical study. J Clin Microbiol. 2020 Jan 28;58:e01643-19.[PubMed Abstract] -
- 74.Lillis RA, Parker RL, Ackerman R, et al. Clinical Evaluation of a New Molecular Test for the Detection of Organisms Causing Vaginitis and Vaginosis. J Clin Microbiol. 2023;61:e0174822.[PubMed Abstract] -
- 75.Larsson PG, Carlsson B. Does pre- and postoperative metronidazole treatment lower vaginal cuff infection rate after abdominal hysterectomy among women with bacterial vaginosis? Infect Dis Obstet Gynecol. 2002;10:133-40.[PubMed Abstract] -
- 76.Larsson PG, Platz-Christensen JJ, Thejls H, Forsum U, Påhlson C. Incidence of pelvic inflammatory disease after first-trimester legal abortion in women with bacterial vaginosis after treatment with metronidazole: a double-blind, randomized study. Am J Obstet Gynecol. 1992;166:100-3.[PubMed Abstract] -
- 77.McElligott KA, Havrilesky LJ, Myers ER. Preoperative screening strategies for bacterial vaginosis prior to elective hysterectomy: a cost comparison study. Am J Obstet Gynecol. 2011;205:500.e1-7.[PubMed Abstract] -
- 78.Penney GC. Preventing infective sequelae of abortion. Hum Reprod. 1997;12:107-12.[PubMed Abstract] -
- 79.Carey JC, Klebanoff MA, Hauth JC, et al. Metronidazole to prevent preterm delivery in pregnant women with asymptomatic bacterial vaginosis. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 2000;342:534-40.[PubMed Abstract] -
- 80.Joesoef MR, Hillier SL, Wiknjosastro G, et al. Intravaginal clindamycin treatment for bacterial vaginosis: effects on preterm delivery and low birth weight. Am J Obstet Gynecol. 1995;173:1527-31.[PubMed Abstract] -
- 83.Vermeulen GM, Bruinse HW. Prophylactic administration of clindamycin 2% vaginal cream to reduce the incidence of spontaneous preterm birth in women with an increased recurrence risk: a randomised placebo-controlled double-blind trial. Br J Obstet Gynaecol. 1999;106:652-7.[PubMed Abstract] -
- 84.Fjeld H, Raknes G. [Is combining metronidazole and alcohol really hazardous?]. Tidsskr Nor Laegeforen. 2014;134:1661-3.[PubMed Abstract] -
- 85.Mergenhagen KA, Wattengel BA, Skelly MK, Clark CM, Russo TA. Fact versus Fiction: a Review of the Evidence behind Alcohol and Antibiotic Interactions. Antimicrob Agents Chemother. 2020;64:e02167-19.[PubMed Abstract] -
- 86.Abad CL, Safdar N. The role of lactobacillus probiotics in the treatment or prevention of urogenital infections--a systematic review. J Chemother. 2009;21:243-52.[PubMed Abstract] -
- 87.Nyirjesy P, Schwebke JR. Secnidazole: next-generation antimicrobial agent for bacterial vaginosis treatment. Future Microbiol. 2018;13:507-24.[PubMed Abstract] -
- 88.Antonio MA, Meyn LA, Murray PJ, Busse B, Hillier SL. Vaginal colonization by probiotic Lactobacillus crispatus CTV-05 is decreased by sexual activity and endogenous Lactobacilli. J Infect Dis. 2009;199:1506-13.[PubMed Abstract] -
- 89.Mastromarino P, Macchia S, Meggiorini L, et al. Effectiveness of Lactobacillus-containing vaginal tablets in the treatment of symptomatic bacterial vaginosis. Clin Microbiol Infect. 2009;15:67-74.[PubMed Abstract] -
- 90.Cohen CR, Wierzbicki MR, French AL, et al. Randomized trial of Lactin-V to prevent recurrence of bacterial vaginosis. N Engl J Med. 2020;382:1906-15.[PubMed Abstract] -
- 91.Marrazzo JM, Antonio M, Agnew K, Hillier SL. Distribution of genital Lactobacillus strains shared by female sex partners. J Infect Dis. 2009;199:680-3.[PubMed Abstract] -
- 92.Burtin P, Taddio A, Ariburnu O, Einarson TR, Koren G. Safety of metronidazole in pregnancy: a meta-analysis. Am J Obstet Gynecol. 1995;172:525-9.[PubMed Abstract] -
- 93.Koss CA, Baras DC, Lane SD, et al. Investigation of metronidazole use during pregnancy and adverse birth outcomes. Antimicrob Agents Chemother. 2012;56:4800-5.[PubMed Abstract] -
- 94.Piper JM, Mitchel EF, Ray WA. Prenatal use of metronidazole and birth defects: no association. Obstet Gynecol. 1993;82:348-52.[PubMed Abstract] -
- 95.Hillier SL, Nyirjesy P, Waldbaum AS, et al. Secnidazole treatment of bacterial vaginosis: a randomized controlled trial. Obstet Gynecol. 2017;130:379-86.[PubMed Abstract] -
- 96.Pentikis H, Adetoro N, Tipping D, Levy S. An Integrated Efficacy and Safety Analysis of Single-Dose Secnidazole 2 g in the Treatment of Bacterial Vaginosis. Reprod Sci. 2020;27:523-8.[PubMed Abstract] -
- 97.Schwebke JR, Morgan FG Jr, Koltun W, Nyirjesy P. A phase-3, double-blind, placebo-controlled study of the effectiveness and safety of single oral doses of secnidazole 2 g for the treatment of women with bacterial vaginosis. Am J Obstet Gynecol. 2017;217:678.e1-678.e9.[PubMed Abstract] -
- 98.Subtil D, Brabant G, Tilloy E, et al. Early clindamycin for bacterial vaginosis in pregnancy (PREMEVA): a multicentre, double-blind, randomised controlled trial. Lancet. 2018;392:2171-9.[PubMed Abstract] -
- 99.Jamieson DJ, Duerr A, Klein RS, et al. Longitudinal analysis of bacterial vaginosis: findings from the HIV epidemiology research study. Obstet Gynecol. 2001;98:656-63.[PubMed Abstract] -
- 100.Bradshaw CS, Brotman RM. Making inroads into improving treatment of bacterial vaginosis - striving for long-term cure. BMC Infect Dis. 2015;15:292.[PubMed Abstract] -
- 101.Sobel JD, Ferris D, Schwebke J, et al. Suppressive antibacterial therapy with 0.75% metronidazole vaginal gel to prevent recurrent bacterial vaginosis. Am J Obstet Gynecol. 2006;194:1283-9.[PubMed Abstract] -
- 102.Muzny CA, Sobel JD. The Role of Antimicrobial Resistance in Refractory and Recurrent Bacterial Vaginosis and Current Recommendations for Treatment. Antibiotics (Basel). 2022;11:500.[PubMed Abstract] -
- 103.Bunge KE, Beigi RH, Meyn LA, Hillier SL. The efficacy of retreatment with the same medication for early treatment failure of bacterial vaginosis. Sex Transm Dis. 2009;36:711-3.[PubMed Abstract] -
- 104.Sobel JD, Sobel R. Current and emerging pharmacotherapy for recurrent bacterial vaginosis. Expert Opin Pharmacother. 2021;22:1593-1600.[PubMed Abstract] -
- 105.Aguin T, Akins RA, Sobel JD. High-dose vaginal maintenance metronidazole for recurrent bacterial vaginosis: a pilot study. Sex Transm Dis. 2014;41:290-1.[PubMed Abstract] -
- 106.Reichman O, Akins R, Sobel JD. Boric acid addition to suppressive antimicrobial therapy for recurrent bacterial vaginosis. Sex Transm Dis. 2009;36:732-4.[PubMed Abstract] -
- 107.McClelland RS, Richardson BA, Hassan WM, et al. Improvement of vaginal health for Kenyan women at risk for acquisition of human immunodeficiency virus type 1: results of a randomized trial. J Infect Dis. 2008;197:1361-8.[PubMed Abstract] -
- 108.Schwebke JR, Carter BA, Waldbaum AS, et al. A phase 3, randomized, controlled trial of Astodrimer 1% Gel for preventing recurrent bacterial vaginosis. Eur J Obstet Gynecol Reprod Biol X. 2021;10:100121.[PubMed Abstract] -
- 109.Van Gerwen OT, Opsteen SA, Graves KJ, Muzny CA. Trichomoniasis. Infect Dis Clin North Am. 2023;37:245-65.[PubMed Abstract] -
- 110.Petrin D, Delgaty K, Bhatt R, Garber G. Clinical and microbiological aspects of Trichomonas vaginalis. Clin Microbiol Rev. 1998;11:300-17.[PubMed Abstract] -
- 111.Cotch MF, Pastorek JG 2nd, Nugent RP, et al. Trichomonas vaginalis associated with low birth weight and preterm delivery. The Vaginal Infections and Prematurity Study Group. Sex Transm Dis. 1997;24:353-60.[PubMed Abstract] -
- 112.Van Gerwen OT, Craig-Kuhn MC, Jones AT, et al. Trichomoniasis and adverse birth outcomes: a systematic review and meta-analysis. BJOG. 2021;128:1907-15.[PubMed Abstract] -
- 113.Yang S, Zhao W, Wang H, Wang Y, Li J, Wu X. Trichomonas vaginalis infection-associated risk of cervical cancer: A meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2018;228:166-173.[PubMed Abstract] -
- 114.Hughes JP, Baeten JM, Lingappa JR, et al. Determinants of per-coital-act HIV-1 infectivity among African HIV-1-serodiscordant couples. J Infect Dis. 2012;205:358-65.[PubMed Abstract] -
- 115.McClelland RS, Sangare L, Hassan WM, et al. Infection with Trichomonas vaginalis increases the risk of HIV-1 acquisition. J Infect Dis. 2007;195:698-702.[PubMed Abstract] -
- 116.Van Der Pol B, Kwok C, Pierre-Louis B, et al. Trichomonas vaginalis infection and human immunodeficiency virus acquisition in African women. J Infect Dis. 2008;197:548-54.[PubMed Abstract] -
- 117.Meites E, Gaydos CA, Hobbs MM, et al. A review of evidence-based care of symptomatic Trichomoniasis and asymptomatic Trichomonas vaginalis infections. Clin Infect Dis. 2015;61 Suppl 8:S837-48.[PubMed Abstract] -
- 118.Hoots BE, Peterman TA, Torrone EA, Weinstock H, Meites E, Bolan GA. A Trich-y question: should Trichomonas vaginalis infection be reportable? Sex Transm Dis. 2013;40:113-6.[PubMed Abstract] -
- 119.Satterwhite CL, Torrone E, Meites E, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis. 2013;40:187-93.[PubMed Abstract] -
- 120.Sutton M, Sternberg M, Koumans EH, McQuillan G, Berman S, Markowitz L. The prevalence of Trichomonas vaginalis infection among reproductive-age women in the United States, 2001-2004. Clin Infect Dis. 2007;45:1319-26.[PubMed Abstract] -
- 121.Flagg EW, Meites E, Phillips C, Papp J, Torrone EA. Prevalence of Trichomonas vaginalis among civilian, noninstitutionalized male and female population aged 14 to 59 years: United States, 2013 to 2016. Sex Transm Dis. 2019;46:e93-e96.[PubMed Abstract] -
- 122.Meites E, Llata E, Braxton J, et al. Trichomonas vaginalis in selected U.S. sexually transmitted disease clinics: testing, screening, and prevalence. Sex Transm Dis. 2013;40:865-9.[PubMed Abstract] -
- 123.Wendel KA, Erbelding EJ, Gaydos CA, Rompalo AM. Use of urine polymerase chain reaction to define the prevalence and clinical presentation of Trichomonas vaginalis in men attending an STD clinic. Sex Transm Infect. 2003;79:151-3.[PubMed Abstract] -
- 124.Schwebke JR, Hook EW 3rd. High rates of Trichomonas vaginalis among men attending a sexually transmitted diseases clinic: implications for screening and urethritis management. J Infect Dis. 2003;188:465-8.[PubMed Abstract] -
- 125.Seña AC, Miller WC, Hobbs MM, et al. Trichomonas vaginalis infection in male sexual partners: implications for diagnosis, treatment, and prevention. Clin Infect Dis. 2007;44:13-22.[PubMed Abstract] -
- 126.Kelley CF, Rosenberg ES, OʼHara BM, Sanchez T, del Rio C, Sullivan PS. Prevalence of urethral Trichomonas vaginalis in black and white men who have sex with men. Sex Transm Dis. 2012;39:739.[PubMed Abstract] -
- 127.Muzny CA, Rivers CA, Mena LA, Schwebke JR. Genotypic characterization of Trichomonas vaginalis isolates among women who have sex with women in sexual partnerships. Sex Transm Dis. 2012;39:556-8.[PubMed Abstract] -
- 128.Rahman N, Ghanem KG, Gilliams E, Page KR, Tuddenham S. Factors associated with sexually transmitted infection diagnosis in women who have sex with women, women who have sex with men and women who have sex with both. Sex Transm Infect. 2021;97:423-8.[PubMed Abstract] -
- 129.Arroyo R, González-Robles A, Martínez-Palomo A, Alderete JF. Signalling of Trichomonas vaginalis for amoeboid transformation and adhesion synthesis follows cytoadherence. Mol Microbiol. 1993;7:299-309.[PubMed Abstract] -
- 130.Alcaide ML, Feaster DJ, Duan R, et al. The incidence of Trichomonas vaginalis infection in women attending nine sexually transmitted diseases clinics in the USA. Sex Transm Infect. 2016;92:58-62.[PubMed Abstract] -
- 131.Swartzendruber A, Sales JM, Brown JL, Diclemente RJ, Rose ES. Correlates of incident Trichomonas vaginalis infections among African American female adolescents. Sex Transm Dis. 2014;41:240-5.[PubMed Abstract] -
- 132.Mayer KH, Bush T, Henry K, et al. Ongoing sexually transmitted disease acquisition and risk-taking behavior among US HIV-infected patients in primary care: implications for prevention interventions. Sex Transm Dis. 2012;39:1-7.[PubMed Abstract] -
- 133.Rogers SM, Turner CF, Hobbs M, et al. Epidemiology of undiagnosed trichomoniasis in a probability sample of urban young adults. PLoS One. 2014;9:e90548.[PubMed Abstract] -
- 134.Fouts AC, Kraus SJ. Trichomonas vaginalis: reevaluation of its clinical presentation and laboratory diagnosis. J Infect Dis. 1980;141:137-143.[PubMed Abstract] -
- 135.Wiringa AE, Ness RB, Darville T, Beigi RH, Haggerty CL. Trichomonas vaginalis, endometritis and sequelae among women with clinically suspected pelvic inflammatory disease. Sex Transm Infect. 2020;96:436-8.[PubMed Abstract] -
- 136.Zhang Z, Li Y, Lu H, et al. A systematic review of the correlation between Trichomonas vaginalis infection and infertility. Acta Trop. 2022;236:106693.[PubMed Abstract] -
- 137.Mann JR, McDermott S, Zhou L, Barnes TL, Hardin J. Treatment of trichomoniasis in pregnancy and preterm birth: an observational study. J Womens Health (Larchmt). 2009;18:493-7.[PubMed Abstract] -
- 138.Mann JR, McDermott S, Gill T. Sexually transmitted infection is associated with increased risk of preterm birth in South Carolina women insured by Medicaid. J Matern Fetal Neonatal Med. 2010;23:563-8.[PubMed Abstract] -
- 139.Carter JE, Whithaus KC. Neonatal respiratory tract involvement by Trichomonas vaginalis: a case report and review of the literature. Am J Trop Med Hyg. 2008;78:17-9.[PubMed Abstract] -
- 140.Trintis J, Epie N, Boss R, Riedel S. Neonatal Trichomonas vaginalis infection: a case report and review of literature. Int J STD AIDS. 2010;21:606-7.[PubMed Abstract] -
- 141.Kissinger P, Adamski A. Trichomoniasis and HIV interactions: a review. Sex Transm Infect. 2013;89:426-33.[PubMed Abstract] -
- 142.Kissinger P, Amedee A, Clark RA, et al. Trichomonas vaginalis treatment reduces vaginal HIV-1 shedding. Sex Transm Dis. 2009;36:11-6.[PubMed Abstract] -
- 143.Moodley P, Wilkinson D, Connolly C, Moodley J, Sturm AW. Trichomonas vaginalis is associated with pelvic inflammatory disease in women infected with human immunodeficiency virus. Clin Infect Dis. 2002;34:519-22.[PubMed Abstract] -
- 144.Masese LN, Graham SM, Gitau R, et al. A prospective study of vaginal trichomoniasis and HIV-1 shedding in women on antiretroviral therapy. BMC Infect Dis. 2011;11:307.[PubMed Abstract] -
- 145.Cu-Uvin S, Ko H, Jamieson DJ, et al. Prevalence, incidence, and persistence or recurrence of trichomoniasis among human immunodeficiency virus (HIV)-positive women and among HIV-negative women at high risk for HIV infection. Clin Infect Dis. 2002;15;34:1406-11.[PubMed Abstract] -
- 146.Schwebke JR, Hobbs MM, Taylor SN, et al. Molecular testing for Trichomonas vaginalis in women: results from a prospective U.S. clinical trial. J Clin Microbiol. 2011;49:4106-11.[PubMed Abstract] -
- 147.Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. Diseases characterized by vaginal itching, burning, irritation, odor or discharge: trichomoniasis. MMWR Recomm Rep. 2021;70(No. RR-4):1-187.
- 148.Kingston MA, Bansal D, Carlin EM. 'Shelf life' of Trichomonas vaginalis. Int J STD AIDS. 2003;14:28-9.[PubMed Abstract] -
- 149.Stoner KA, Rabe LK, Meyn LA, Hillier SL. Survival of Trichomonas vaginalis in wet preparation and on wet mount. Sex Transm Infect. 2013;89:485-8.[PubMed Abstract] -
- 150.Cosentino LA, Campbell T, Jett A, et al. Use of nucleic acid amplification testing for diagnosis of anorectal sexually transmitted infections. J Clin Microbiol. 2012;50:2005-8.[PubMed Abstract] -
- 151.Francis SC, Kent CK, Klausner JD, et al. Prevalence of rectal Trichomonas vaginalis and Mycoplasma genitalium in male patients at the San Francisco STD clinic, 2005-2006. Sex Transm Dis. 2008;35:797-800.[PubMed Abstract] -
- 152.Chapin K, Andrea S. APTIMA® Trichomonas vaginalis, a transcription-mediated amplification assay for detection of Trichomonas vaginalis in urogenital specimens. Expert Rev Mol Diagn. 2011;11:679-88.[PubMed Abstract] -
- 153.Association of Public Health Laboratories. Advances in the laboratory detection of Trichomonas vaginalis. August 2013.[APHL] -
- 154.Hollman D, Coupey SM, Fox AS, Herold BC. Screening for Trichomonas vaginalis in high-risk adolescent females with a new transcription-mediated nucleic acid amplification test (NAAT): associations with ethnicity, symptoms, and prior and current STIs. J Pediatr Adolesc Gynecol. 2010;23:312-6.[PubMed Abstract] -
- 155.Andrea SB, Chapin KC. Comparison of Aptima Trichomonas vaginalis transcription-mediated amplification assay and BD affirm VPIII for detection of T. vaginalis in symptomatic women: performance parameters and epidemiological implications. J Clin Microbiol. 2011;49:866-9.[PubMed Abstract] -
- 156.Nye MB, Schwebke JR, Body BA. Comparison of APTIMA Trichomonas vaginalis transcription-mediated amplification to wet mount microscopy, culture, and polymerase chain reaction for diagnosis of trichomoniasis in men and women. Am J Obstet Gynecol. 2009;200:188.e1-7.[PubMed Abstract] -
- 157.Van Der Pol B, Williams JA, Taylor SN, et al. Detection of Trichomonas vaginalis DNA by use of self-obtained vaginal swabs with the BD ProbeTec Qx assay on the BD Viper system. J Clin Microbiol. 2014;52:885-9.[PubMed Abstract] -
- 158.Schwebke JR, Gaydos CA, Davis T, et al. Clinical Evaluation of the Cepheid Xpert TV Assay for Detection of Trichomonas vaginalis with Prospectively Collected Specimens from Men and Women. J Clin Microbiol. 2018;56:e01091-17.[PubMed Abstract] -
- 159.Van Der Pol B, Torres-Chavolla E, Kodsi S, et al. Clinical Performance of the BD CTGCTV2 Assay for the BD MAX System for detection of Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis infections. Sex Transm Dis. 2021;48:134-40.[PubMed Abstract] -
- 160.Van Der Pol B. A profile of the cobas® TV/ MG test for the detection of Trichomonas vaginalis and Mycoplasma genitalium. Expert Rev Mol Diagn. 2020;20:381-6.[PubMed Abstract] -
- 161.Van Der Pol B, Rao A, Nye MB, et al. Trichomonas vaginalis detection in urogenital specimens from symptomatic and asymptomatic men and women by use of the cobas TV/MG Test. J Clin Microbiol. 2021;59:e0026421.[PubMed Abstract] -
- 162.Matysiak C, Cheng A, Kirby JE. Evaluation of the Abbott Alinity m STI assay for diagnosis of the primary causes of sexually transmitted infections in the United States. Pract Lab Med. 2023;36:e00332.[PubMed Abstract] -
- 163.Lima A, Uy D, Kostera J, Silbert S. Clinical Evaluation of the Alinity m STI Multiplex PCR Assay. Sex Transm Dis. 2024;51:480-5.[PubMed Abstract] -
- 164.Gaydos CA, Manabe YC, Melendez JH. A Narrative Review of Where We Are With Point-of-Care Sexually Transmitted Infection Testing in the United States. Sex Transm Dis. 2021;48:S71-S77.[PubMed Abstract] -
- 165.Sheele JM, Crandall CJ, Arko BL, et al. The OSOM® Trichomonas Test is unable to accurately diagnose Trichomonas vaginalis from urine in men. Am J Emerg Med. 2019;37:1002-3.[PubMed Abstract] -
- 166.Campbell L, Woods V, Lloyd T, Elsayed S, Church DL. Evaluation of the OSOM Trichomonas rapid test versus wet preparation examination for detection of Trichomonas vaginalis vaginitis in specimens from women with a low prevalence of infection. J Clin Microbiol. 2008;46:3467-9.[PubMed Abstract] -
- 167.Gaydos CA, Schwebke J, Dombrowski J, et al. Clinical performance of the Solana® Point-of-Care Trichomonas Assay from clinician-collected vaginal swabs and urine specimens from symptomatic and asymptomatic women. Expert Rev Mol Diagn. 2017;17:303-6.[PubMed Abstract] -
- 168.Morris SR, Bristow CC, Wierzbicki MR, et al. Performance of a single-use, rapid, point-of-care PCR device for the detection of Neisseria gonorrhoeae, Chlamydia trachomatis, and Trichomonas vaginalis: a cross-sectional study. Lancet Infect Dis. 2021;21:668-76.[PubMed Abstract] -
- 169.Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. Screening recommendations and considerations referenced in treatment guidelines and original sources. MMWR Recomm Rep. 2021;70(No. RR-4):1-187.
- 170.Howe K, Kissinger PJ. Single-dose compared with multidose metronidazole for the treatment of trichomoniasis in women: a meta-analysis. Sex Transm Dis. 2017;44:29-34.[PubMed Abstract] -
- 171.Kissinger P, Muzny CA, Mena LA, et al. Single-dose versus 7-day-dose metronidazole for the treatment of trichomoniasis in women: an open-label, randomised controlled trial. Lancet Infect Dis. 2018;18:1251-9.[PubMed Abstract] -
- 172.Muzny CA, Van Gerwen OT. Secnidazole for Trichomoniasis in Women and Men. Sex Med Rev. 2022;10:255-62.[PubMed Abstract] -
- 173.Muzny CA, Van Gerwen OT, Legendre D. Secnidazole: a treatment for trichomoniasis in adolescents and adults. Expert Rev Anti Infect Ther. 2022;20:1067-76.[PubMed Abstract] -
- 174.Muzny CA, Schwebke JR, Nyirjesy P, et al. Efficacy and Safety of Single Oral Dosing of Secnidazole for Trichomoniasis in Women: Results of a Phase 3, Randomized, Double-Blind, Placebo-Controlled, Delayed-Treatment Study. Clin Infect Dis. 2021;73:e1282-e1289.[PubMed Abstract] -
- 175.Helms DJ, Mosure DJ, Secor WE, Workowski KA. Management of Trichomonas vaginalis in women with suspected metronidazole hypersensitivity. Am J Obstet Gynecol. 2008;198:370.e1-7.[PubMed Abstract] -
- 176.Muzny C, Barnes A, Mena L. Symptomatic Trichomonas vaginalis infection in the setting of severe nitroimidazole allergy: successful treatment with boric acid. Sex Health. 2012;9:389-91.[PubMed Abstract] -
- 177.Nyirjesy P, Gilbert J, Mulcahy LJ. Resistant trichomoniasis: successful treatment with combination therapy. Sex Transm Dis. 2011;38:962-3.[PubMed Abstract] -
- 178.Kirkcaldy RD, Augostini P, Asbel LE, et al. Trichomonas vaginalis antimicrobial drug resistance in 6 US cities, STD Surveillance Network, 2009-2010. Emerg Infect Dis. 2012;18:939-43.[PubMed Abstract] -
- 179.Schwebke JR, Barrientes FJ. Prevalence of Trichomonas vaginalis isolates with resistance to metronidazole and tinidazole. Antimicrob Agents Chemother. 2006;50:4209-10.[PubMed Abstract] -
- 180.Bosserman EA, Helms DJ, Mosure DJ, Secor WE, Workowski KA. Utility of antimicrobial susceptibility testing in Trichomonas vaginalis-infected women with clinical treatment failure. Sex Transm Dis. 2011;38:983-7.[PubMed Abstract] -
- 181.Sobel JD, Nyirjesy P, Brown W. Tinidazole therapy for metronidazole-resistant vaginal trichomoniasis. Clin Infect Dis. 2001;33:1341-6.[PubMed Abstract] -
- 182.McNeil CJ, Williamson JC, Muzny CA. Successful Treatment of Persistent 5-Nitroimidazole-Resistant Trichomoniasis With an Extended Course of Oral Secnidazole Plus Intravaginal Boric Acid. Sex Transm Dis. 2023;50:243-6.[PubMed Abstract] -
- 183.Van Gerwen OT, Camino AF, Bourla LN, Legendre D, Muzny CA. Management of trichomoniasis in the setting of 5-nitroimidazole hypersensitivity. Sex Transm Dis. 2021;48:e111-e115.[PubMed Abstract] -
- 184.Klebanoff MA, Carey JC, Hauth JC, et al. Failure of metronidazole to prevent preterm delivery among pregnant women with asymptomatic Trichomonas vaginalis infection. N Engl J Med. 2001;345:487-93.[PubMed Abstract] -
- 185.Erickson SH, Oppenheim GL, Smith GH. Metronidazole in breast milk. Obstet Gynecol. 1981;57:48-50.[PubMed Abstract] -
- 186.Kissinger P, Mena L, Levison J, et al. A randomized treatment trial: single versus 7-day dose of metronidazole for the treatment of Trichomonas vaginalis among HIV-infected women. J Acquir Immune Defic Syndr. 2010;55:565-71.[PubMed Abstract] -
- 187.Kissinger P, Adamski A, Clark RA, Mena L, Levison J, Martin DH. Does antiretroviral therapy interfere with the treatment of Trichomonas vaginalis among HIV+ women? Sex Transm Dis. 2013;40:506-7.[PubMed Abstract] -
- 188.Balkus JE, Richardson BA, Mochache V, et al. A prospective cohort study comparing the effect of single-dose 2 g metronidazole on Trichomonas vaginalis infection in HIV-seropositive versus HIV-seronegative women. Sex Transm Dis. 2013;40:499-505.[PubMed Abstract] -
- 189.Pintye J, Drake AL, Unger JA, et al. Male partner circumcision associated with lower Trichomonas vaginalis incidence among pregnant and postpartum Kenyan women: a prospective cohort study. Sex Transm Infect. 2017;93:137-43.[PubMed Abstract] -
- 190.Bochner AF, Baeten JM, Rustagi AS, et al. A cross-sectional analysis of Trichomonas vaginalis infection among heterosexual HIV-1 serodiscordant African couples. Sex Transm Infect. 2017;93:520-9.[PubMed Abstract] -
- 191.Denning DW, Kneale M, Sobel JD, Rautemaa-Richardson R. Global burden of recurrent vulvovaginal candidiasis: a systematic review. Lancet Infect Dis. 2018;18:e339-e47.[PubMed Abstract] -
- 192.Sobel JD. Vulvovaginal candidosis. Lancet. 2007;369:1961-71.[PubMed Abstract] -
- 193.Gonçalves B, Ferreira C, Alves CT, Henriques M, Azeredo J, Silva S. Vulvovaginal candidiasis: Epidemiology, microbiology and risk factors. Crit Rev Microbiol. 2016;42:905-27.[PubMed Abstract] -
- 194.Sobel JD, Wiesenfeld HC, Martens M, et al. Maintenance fluconazole therapy for recurrent vulvovaginal candidiasis. N Engl J Med. 2004;351:876-83.[PubMed Abstract] -
- 195.Eckert LO, Hawes SE, Stevens CE, Koutsky LA, Eschenbach DA, Holmes KK. Vulvovaginal candidiasis: clinical manifestations, risk factors, management algorithm. Obstet Gynecol. 1998;92:757-65.[PubMed Abstract] -
- 196.Anderson BL, Firnhaber C, Liu T, et al. Effect of trichomoniasis therapy on genital HIV viral burden among African women. Sex Transm Dis. 2012;39:638-42.[PubMed Abstract] -
- 197.Duerr A, Heilig CM, Meikle SF, et al. Incident and persistent vulvovaginal candidiasis among human immunodeficiency virus-infected women: Risk factors and severity. Obstet Gynecol. 2003;101:548-56.[PubMed Abstract] -
- 198.Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. Diseases characterized by vaginal itching, burning, irritation, odor or discharge: vulvovaginal candidiasis. MMWR Recomm Rep. 2021;70(No. RR-4):1-187.
- 199.Marchaim D, Lemanek L, Bheemreddy S, Kaye KS, Sobel JD. Fluconazole-resistant Candida albicans vulvovaginitis. Obstet Gynecol. 2012;120:1407-14.[PubMed Abstract] -
- 200.Shahid Z, Sobel JD. Reduced fluconazole susceptibility of Candida albicans isolates in women with recurrent vulvovaginal candidiasis: effects of long-term fluconazole therapy. Diagn Microbiol Infect Dis. 2009;64:354-6.[PubMed Abstract] -
- 201.Ilkit M, Guzel AB. The epidemiology, pathogenesis, and diagnosis of vulvovaginal candidosis: a mycological perspective. Crit Rev Microbiol. 2011;37:250-61.[PubMed Abstract] -
- 202.Sobel JD, Faro S, Force RW, et al. Vulvovaginal candidiasis: epidemiologic, diagnostic, and therapeutic considerations. Am J Obstet Gynecol. 1998;178:203-11.[PubMed Abstract] -
- 203.Schwebke JR, Sobel R, Gersten JK, et al. Ibrexafungerp Versus Placebo for Vulvovaginal Candidiasis Treatment: A Phase 3, Randomized, Controlled Superiority Trial (VANISH 303). Clin Infect Dis. 2022;74:1979-85.[PubMed Abstract] -
- 204.Sobel R, Nyirjesy P, Ghannoum MA, et al. Efficacy and safety of oral ibrexafungerp for the treatment of acute vulvovaginal candidiasis: a global phase 3, randomised, placebo-controlled superiority study (VANISH 306). BJOG. 2022;129:412-20.[PubMed Abstract] -
- 205.Aridogan IA, Izol V, Ilkit M. Superficial fungal infections of the male genitalia: a review. Crit Rev Microbiol. 2011;37:237-44.[PubMed Abstract] -
- 206.Stary A, Soeltz-Szoets J, Ziegler C, Kinghorn GR, Roy RB. Comparison of the efficacy and safety of oral fluconazole and topical clotrimazole in patients with candida balanitis. Genitourin Med. 1996;72:98-102.[PubMed Abstract] -
- 207.Martens MG, Maximos B, Degenhardt T, et al. Phase 3 study evaluating the safety and efficacy of oteseconazole in the treatment of recurrent vulvovaginal candidiasis and acute vulvovaginal candidiasis infections. Am J Obstet Gynecol. 2022;227:880.e1-880.e11.[PubMed Abstract] -
- 208.Sobel JD, Donders G, Degenhardt T, et al. Efficacy and Safety of Oteseconazole in Recurrent Vulvovaginal Candidiasis. NEJM Evid. 2022;1:EVIDoa2100055.[PubMed Abstract] -
- 209.Phillips NA, Rocktashel M, Merjanian L. Ibrexafungerp for the Treatment of Vulvovaginal Candidiasis: Design, Development and Place in Therapy. Drug Des Devel Ther. 2023;17:363-7.[PubMed Abstract] -
- 210.Kennedy MA, Sobel JD. Vulvovaginal candidiasis caused by non-albicans Candida species: new insights. Curr Infect Dis Rep. 2010;12:465-70.[PubMed Abstract] -
- 211.Sobel JD, Chaim W, Nagappan V, Leaman D. Treatment of vaginitis caused by Candida glabrata: use of topical boric acid and flucytosine. Am J Obstet Gynecol. 2003;189:1297-300.[PubMed Abstract] -
- 212.Panel on Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Candidiasis (Mucocutaneous). May 26, 2020.[HIV.gov] -
- 213.Mølgaard-Nielsen D, Pasternak B, Hviid A. Use of oral fluconazole during pregnancy and the risk of birth defects. N Engl J Med. 2013;369:830-9.[PubMed Abstract] -
- 214.Bérard A, Sheehy O, Zhao JP, et al. Associations between low- and high-dose oral fluconazole and pregnancy outcomes: 3 nested case-control studies. CMAJ. 2019;191:E179-E187.[PubMed Abstract] -
- 215.Sucher AJ, Thai A, Tran C, Mantena N, Noronha A, Chahine EB. Ibrexafungerp: A new triterpenoid antifungal. Am J Health Syst Pharm. 2022;79:2208-21.[PubMed Abstract] -
Additional References
- Abd El Aziz MA, Sharifipour F, Abedi P, Jahanfar S, Judge HM. Secnidazole for treatment of bacterial vaginosis: a systematic review. BMC Womens Health. 2019;19:121.[PubMed Abstract] -
- Balkus JE, Manhart LE, Lee J, et al. Periodic Presumptive Treatment for Vaginal Infections May Reduce the Incidence of Sexually Transmitted Bacterial Infections. J Infect Dis. 2016;213:1932-7.[PubMed Abstract] -
- Gaydos CA, Hobbs M, Marrazzo J, et al. Rapid diagnosis of Trichomonas vaginalis by testing vaginal swabs in an isothermal helicase-dependent AmpliVue assay. Sex Transm Dis. 2016;43:369-73.[PubMed Abstract] -
- Lord E, Newnham T, Dorrell L, et al. Detecting asymptomatic Trichomonas vaginalis in females using the BD ProbeTec™ Trichomonas vaginalis Qx nucleic acid amplification test. Int J STD AIDS. 2016:8:357-61.[PubMed Abstract] -
- Martin DH, Marrazzo JM. The vaginal microbiome: current understanding and future directions. J Infect Dis. 2016;214 Suppl 1:S36-41.[PubMed Abstract] -
- Muzny CA, Sunesara IR, Martin DH, Mena LA. Sexually transmitted infections and risk behaviors among African American women who have sex with women: does sex with men make a difference? Sex Transm Dis. 2011;38:1118-25.[PubMed Abstract] -
- Najafi A, Chaechi Nosrati MR, Ghasemi E, et al. Is there association between Trichomonas vaginalis infection and prostate cancer risk?: A systematic review and meta-analysis. Microb Pathog. 2019;137:103752.[PubMed Abstract] -
- Petrina MAB, Cosentino LA, Rabe LK, Hillier SL. Susceptibility of bacterial vaginosis (BV)-associated bacteria to secnidazole compared to metronidazole, tinidazole and clindamycin. Anaerobe. 2017;47:115-119.[PubMed Abstract] -
- Schwebke JR, Hillier SL, Sobel JD, McGregor JA, Sweet RL. Validity of the vaginal gram stain for the diagnosis of bacterial vaginosis. Obstet Gynecol. 1996;88:573-6.[PubMed Abstract] -
- Schwebke JR, Lee JY, Lensing S, et al. Home Screening for Bacterial Vaginosis to Prevent Sexually Transmitted Diseases. Clin Infect Dis. 2016;62:531-6.[PubMed Abstract] -
- Schwebke JR, Muzny CA, Josey WE. Role of Gardnerella vaginalis in the pathogenesis of bacterial vaginosis: a conceptual model. J Infect Dis. 2014;210:338-43.[PubMed Abstract] -
- Seña AC, Bachmann LH, Hobbs MM. Persistent and recurrent Trichomonas vaginalis infections: epidemiology, treatment and management considerations. Expert Rev Anti Infect Ther. 2014;12:673-85.[PubMed Abstract] -
- Tayal SC, Ochogwu SA, Bunce H. Paromomycin treatment of recalcitrant Trichomonas vaginalis. Int J STD AIDS. 2010;21:217-8.[PubMed Abstract] -
- Zozaya M, Ferris MJ, Siren JD, et al. Bacterial communities in penile skin, male urethra, and vaginas of heterosexual couples with and without bacterial vaginosis. Microbiome. 2016;4:16.[PubMed Abstract] -
Figures
 Figure 1 (Image Series). Prevalence of Bacterial Vaginosis in the United States, 2001–2004Source: Koumans EH, Sternberg M, Bruce C, et al. The prevalence of bacterial vaginosis in the United States, 2001-2004; associations with symptoms, sexual behaviors, and reproductive health. Sex Transm Dis. 2007;34:864-9.
Figure 1 (Image Series). Prevalence of Bacterial Vaginosis in the United States, 2001–2004Source: Koumans EH, Sternberg M, Bruce C, et al. The prevalence of bacterial vaginosis in the United States, 2001-2004; associations with symptoms, sexual behaviors, and reproductive health. Sex Transm Dis. 2007;34:864-9. Figure 1B. Prevalence and Frequency of Vaginal Douching in Prior 6 MonthsSource: Koumans EH, Sternberg M, Bruce C, et al. The prevalence of bacterial vaginosis in the United States, 2001-2004; associations with symptoms, sexual behaviors, and reproductive health. Sex Transm Dis. 2007;34:864-9.
Figure 1B. Prevalence and Frequency of Vaginal Douching in Prior 6 MonthsSource: Koumans EH, Sternberg M, Bruce C, et al. The prevalence of bacterial vaginosis in the United States, 2001-2004; associations with symptoms, sexual behaviors, and reproductive health. Sex Transm Dis. 2007;34:864-9. Figure 2. Bacterial Vaginosis—Clue CellsThis illustration shows a wet mount saline microscopic examination of a vaginal smear. The clue cells on the right are vaginal epithelial cells covered with abundant bacteria.Illustration: Cognition Studio, Inc. and David H. Spach, MD
Figure 2. Bacterial Vaginosis—Clue CellsThis illustration shows a wet mount saline microscopic examination of a vaginal smear. The clue cells on the right are vaginal epithelial cells covered with abundant bacteria.Illustration: Cognition Studio, Inc. and David H. Spach, MD Figure 3 (Image Series). Nugent Scoring SystemThe Nugent scoring is based on morphotypes per high power field of a gram-stained vaginal swab sample.Source: Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29:297-301.
Figure 3 (Image Series). Nugent Scoring SystemThe Nugent scoring is based on morphotypes per high power field of a gram-stained vaginal swab sample.Source: Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29:297-301. Figure 3B. Nugent Score = 04+ Lactobacillus morphotypes, no small gram-negative or gram-variable rods (score = 0);Source: Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29:297-301. Reproduced with permission from the American Society of Microbiology.
Figure 3B. Nugent Score = 04+ Lactobacillus morphotypes, no small gram-negative or gram-variable rods (score = 0);Source: Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29:297-301. Reproduced with permission from the American Society of Microbiology. Figure 3C. Nugent Score = 23+ Lactobacillus morphotypes, 1+ Gardnerella spp. morphotypes (score = 2);Source: Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29:297-301. Reproduced with permission from the American Society of Microbiology.
Figure 3C. Nugent Score = 23+ Lactobacillus morphotypes, 1+ Gardnerella spp. morphotypes (score = 2);Source: Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29:297-301. Reproduced with permission from the American Society of Microbiology. Figure 3D. Nugent Score = 43+ Lactobacillus morphotypes and 3+ small gram-variable rods (score = 4);Source: Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29:297-301. Reproduced with permission from the American Society of Microbiology.
Figure 3D. Nugent Score = 43+ Lactobacillus morphotypes and 3+ small gram-variable rods (score = 4);Source: Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29:297-301. Reproduced with permission from the American Society of Microbiology. Figure 3E. Nugent Score = 62+ Lactobacillus morphotypes and 4+ small gram-negative and gram-variable rods (score = 6)Source: Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29:297-301. Reproduced with permission from the American Society of Microbiology.
Figure 3E. Nugent Score = 62+ Lactobacillus morphotypes and 4+ small gram-negative and gram-variable rods (score = 6)Source: Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29:297-301. Reproduced with permission from the American Society of Microbiology. Figure 3F. Nugent Score = 8No lactobacilli and 4+ gram-negative and gram-variable rods (score = 8)
Figure 3F. Nugent Score = 8No lactobacilli and 4+ gram-negative and gram-variable rods (score = 8)
Note clue cell on leftSource: Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29:297-301. Reproduced with permission from the American Society of Microbiology. Figure 3G. Nugent Score = 10No lactobacilli and 4+ gram-negative rods and curved rods (score = 10)
Figure 3G. Nugent Score = 10No lactobacilli and 4+ gram-negative rods and curved rods (score = 10)
Note the Mobiluncus spp. morphotypes on the clue cell (center of field).Source: Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29:297-301. Reproduced with permission from the American Society of Microbiology. Figure 4. Performance of BD-MAX Vaginal Panel for the Diagnosis of Bacterial VaginosisSource: Gaydos CA, Beqaj S, Schwebke JR, et al. Clinical validation of a test for the diagnosis of vaginitis. Obstet Gynecol. 2017;130:181-9.
Figure 4. Performance of BD-MAX Vaginal Panel for the Diagnosis of Bacterial VaginosisSource: Gaydos CA, Beqaj S, Schwebke JR, et al. Clinical validation of a test for the diagnosis of vaginitis. Obstet Gynecol. 2017;130:181-9. Figure 5. Performance of Aptima Vaginal Panel for the Diagnosis of Bacterial VaginosisSource: Schwebke JR, Taylor SN, Ackerman R, et al. Clinical validation of the Aptima bacterial vaginosis and Aptima Candida/Trichomonas vaginitis assays: results from a prospective multicenter clinical study. J Clin Microbiol. 2020;58:e01643-19.
Figure 5. Performance of Aptima Vaginal Panel for the Diagnosis of Bacterial VaginosisSource: Schwebke JR, Taylor SN, Ackerman R, et al. Clinical validation of the Aptima bacterial vaginosis and Aptima Candida/Trichomonas vaginitis assays: results from a prospective multicenter clinical study. J Clin Microbiol. 2020;58:e01643-19. Figure 6. Prevalence of Trichomonas vaginalis Among Civilian, Noninstitutionalized Females Aged 14 to 59 Years: United States, 2013 to 2016Source: Flagg EW, Meites E, Phillips C, Papp J, Torrone EA. Prevalence of Trichomonas vaginalis among civilian, noninstitutionalized male and female population aged 14 to 59 years: United States, 2013 to 2016. Sex Transm Dis. 2019;46:e93-e96.
Figure 6. Prevalence of Trichomonas vaginalis Among Civilian, Noninstitutionalized Females Aged 14 to 59 Years: United States, 2013 to 2016Source: Flagg EW, Meites E, Phillips C, Papp J, Torrone EA. Prevalence of Trichomonas vaginalis among civilian, noninstitutionalized male and female population aged 14 to 59 years: United States, 2013 to 2016. Sex Transm Dis. 2019;46:e93-e96. Figure 7. Trichomonas vaginalisTrichomonas vaginalis is a pear-shaped flagellated protozoan parasitic organism that is approximately 10 by 7 micrometers. The organism achieves a quivering motion via the anterior flagella and the undulating membrane. After attaching to vaginal epithelial cells, the organism takes on a more ameboid-like appearance.Illustration: Cognition Studio, Inc. and David H. Spach, MD
Figure 7. Trichomonas vaginalisTrichomonas vaginalis is a pear-shaped flagellated protozoan parasitic organism that is approximately 10 by 7 micrometers. The organism achieves a quivering motion via the anterior flagella and the undulating membrane. After attaching to vaginal epithelial cells, the organism takes on a more ameboid-like appearance.Illustration: Cognition Studio, Inc. and David H. Spach, MD Figure 8 (Image Series). Cervical Abnormalities with TrichomoniasisIllustration: Cognition Studio, Inc. and David H. Spach, MD
Figure 8 (Image Series). Cervical Abnormalities with TrichomoniasisIllustration: Cognition Studio, Inc. and David H. Spach, MD Figure 8B. Cervical Petechiae with TrichomoniasisThis illustration shows multiple petechiae on the cervix surrounding the cervical os.Illustration: Cognition Studio, Inc. and David H. Spach, MD
Figure 8B. Cervical Petechiae with TrichomoniasisThis illustration shows multiple petechiae on the cervix surrounding the cervical os.Illustration: Cognition Studio, Inc. and David H. Spach, MD Figure 8C. Trichomoniasis and Cervical PetechiaeThis photograph shows multiple petechiae on the cervix of a woman with trichomoniasis. This suggests a diagnosis of trichomoniasis and is often referred to as a "strawberry cervix".Source: Claire Stevens, University of Washington
Figure 8C. Trichomoniasis and Cervical PetechiaeThis photograph shows multiple petechiae on the cervix of a woman with trichomoniasis. This suggests a diagnosis of trichomoniasis and is often referred to as a "strawberry cervix".Source: Claire Stevens, University of Washington Figure 9. Trichomonas vaginalis on Wet MountThis photomicrograph taken of a vaginal discharge wet mount sample shows numerous oval Trichomonas vaginalis protozoan parasites; the black arrow on left indicates two characteristic T. vaginalis organisms (the thin flagellum can be faintly seen).Source: Centers for Disease Control and Prevention Public Health Image Library (Joe Miller, 1975).
Figure 9. Trichomonas vaginalis on Wet MountThis photomicrograph taken of a vaginal discharge wet mount sample shows numerous oval Trichomonas vaginalis protozoan parasites; the black arrow on left indicates two characteristic T. vaginalis organisms (the thin flagellum can be faintly seen).Source: Centers for Disease Control and Prevention Public Health Image Library (Joe Miller, 1975).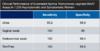 Figure 10. Performance of Aptima for Diagnosis of TrichomonasAmong the women enrolled, 60% were symptomatic, most often with vaginal discharge.Source: Schwebke JR, Hobbs MM, Taylor SN, et al. Molecular testing for Trichomonas vaginalis in women: results from a prospective U.S. clinical trial. J Clin Microbiol. 2011;49:4106-11.
Figure 10. Performance of Aptima for Diagnosis of TrichomonasAmong the women enrolled, 60% were symptomatic, most often with vaginal discharge.Source: Schwebke JR, Hobbs MM, Taylor SN, et al. Molecular testing for Trichomonas vaginalis in women: results from a prospective U.S. clinical trial. J Clin Microbiol. 2011;49:4106-11. Figure 11. Treatment of Trichomoniasis in Women with HIVSource: Kissinger P, Mena L, Levison J, et al. A randomized treatment trial: single versus 7-day dose of metronidazole for the treatment of Trichomonas vaginalis among HIV-infected women. J Acquir Immune Defic Syndr. 2010;55:565-71.
Figure 11. Treatment of Trichomoniasis in Women with HIVSource: Kissinger P, Mena L, Levison J, et al. A randomized treatment trial: single versus 7-day dose of metronidazole for the treatment of Trichomonas vaginalis among HIV-infected women. J Acquir Immune Defic Syndr. 2010;55:565-71. Figure 12. Candida albicans Yeast and Hyphae FormsIllustration with 3D rendering of Candida albicans showing yeast and hyphae forms.Illustration by 306/Shutterstock.com. Image used under license from Shutterstock.com.
Figure 12. Candida albicans Yeast and Hyphae FormsIllustration with 3D rendering of Candida albicans showing yeast and hyphae forms.Illustration by 306/Shutterstock.com. Image used under license from Shutterstock.com. Figure 13. Vulvovaginal Candidiasis—Intravaginal ViewThis photograph was taken during a pelvic examination with a speculum inserted into the vagina. There are thick white clumps visible on the cervix (image center) and vaginal wall.Source: Public Health—Seattle & King County Sexual Health Clinic
Figure 13. Vulvovaginal Candidiasis—Intravaginal ViewThis photograph was taken during a pelvic examination with a speculum inserted into the vagina. There are thick white clumps visible on the cervix (image center) and vaginal wall.Source: Public Health—Seattle & King County Sexual Health Clinic Figure 14 (Image Series). Vaginal Wet Mount for Diagnosing Vulvovaginal CandidiasisThis photograph is taken of a vaginal wet mount sample that has been prepared with 10% potassium hydroxide. Abundant yeasts and hyphae are visible in a tangled mass. Magnification 10x.Source: Public Health—Seattle & King County Sexual Health Clinic
Figure 14 (Image Series). Vaginal Wet Mount for Diagnosing Vulvovaginal CandidiasisThis photograph is taken of a vaginal wet mount sample that has been prepared with 10% potassium hydroxide. Abundant yeasts and hyphae are visible in a tangled mass. Magnification 10x.Source: Public Health—Seattle & King County Sexual Health Clinic Figure 14B. Saline Vaginal Wet MountThis photograph taken of a saline vaginal wet mount sample shows multiple yeast forms (blue arrows) and hyphae forms (red arrow on right). Magnification 40x.Source: Public Health—Seattle & King County Sexual Health Clinic
Figure 14B. Saline Vaginal Wet MountThis photograph taken of a saline vaginal wet mount sample shows multiple yeast forms (blue arrows) and hyphae forms (red arrow on right). Magnification 40x.Source: Public Health—Seattle & King County Sexual Health ClinicTables
Table 1. 2021 STI Treatment Guidelines: Bacterial VaginosisTreatment of Bacterial VaginosisRecommended RegimensMetronidazole500 mg orally twice a day for 7 daysMetronidazole
Tradename:FlagylRecommended RegimensMetronidazole gel 0.75%one full applicator (5 g) intravaginally, once a day for 5 daysMetronidazole gel 0.75%
Tradename:Recommended RegimensClindamycin vaginal cream 2%one full applicator (5 g) intravaginally at bedtime for 7 daysClindamycin vaginal cream 2%
Tradename:Cleocin vaginal creamNote: Clindamycin cream is oil based and might weaken latex condoms and diaphragms for 5 days after use.Alternative RegimensClindamycin300 mg orally twice daily for 7 daysClindamycin
Tradename:CleocinAlternative RegimensClindamycin ovules100 mg intravaginally once at bedtime for 3 daysClindamycin ovules
Tradename:Note: Clindamycin ovules use an oleaginous base that might weaken latex or rubber products (e.g. condoms and diaphragms). Use of such products within 72 hours after treatment with clindamycin ovules is not recommended.Alternative RegimensSecnidazole2 g oral granules in a single doseSecnidazole
Tradename:SolosecNote: Oral granules should be sprinkled onto unsweetened applesauce, yogurt, or pudding before ingestion. A glass of water can be taken after administration to aid in swallowing.Alternative RegimensTinidazole2 g orally once daily for 2 daysTinidazole
Tradename:TindamaxAlternative RegimensTinidazole1 g orally once daily for 5 daysTinidazole
Tradename:TindamaxSource: Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. Diseases characterized by vaginal itching, burning, irritation, odor or discharge: bacterial vaginosis. MMWR Recomm Rep. 2021;70(No. RR-4):1-187. [2021 STI Treatment Guidelines]Table 2. 2021 STI Treatment Guidelines: TrichomoniasisTreatment of TrichomoniasisRecommended Regimen for WomenMetronidazole500 mg orally twice a day for 7 daysMetronidazole
Tradename:FlagylRecommended Regimen for MenMetronidazole2 g orally in a single doseMetronidazole
Tradename:FlagylAlternative Regimen for Women and MenTinidazole2 g orally in a single doseTinidazole
Tradename:TindamaxSource: Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. Diseases characterized by vaginal itching, burning, irritation, odor or discharge: trichomoniasis. MMWR Recomm Rep. 2021;70(No. RR-4):1-187. [2021 STI Treatment Guidelines]Table 3. Classification of Vulvovaginal Candidiasis
Abbreviation: HIV = human immunodeficiency virus. Uncomplicated Vulvovaginal Candidiasis
- Sporadic or infrequent vulvovaginal candidiasis
and
- Mild-to-moderate vulvovaginal candidiasis
and
- Likely to be Candida albicans
and
- Nonimmunocompromised women
Complicated Vulvovaginal Candidiasis
- Recurrent vulvovaginal candidiasis (three or more episodes of symptomatic vulvovaginal candidiasis in <1 year)
or
- Severe vulvovaginal candidiasis
or
- Non-albicans candidiasis
or
- Women with diabetes, immunocompromising conditions (e.g., HIV), underlying immunodeficiency, or immunosuppressive therapy (e.g., corticosteroids)
Source:- Sobel JD, Faro S, Force RW, et al. Vulvovaginal candidiasis: epidemiologic, diagnostic, and therapeutic considerations. Am J Obstet Gynecol. 1998;178:203-11. [PubMed Abstract]
- Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. Diseases characterized by vaginal itching, burning, irritation, odor or discharge: vulvovaginal candidiasis. MMWR Recomm Rep. 2021;70(No. RR-4):1-187. [2021 STI Treatment Guidelines]
Table 4. 2021 STI Treatment Guidelines: Vulvovaginal CandidiasisTreatment of Uncomplicated Vulvovaginal CandidiasisRecommended Regimens: Over-the-Counter Intravaginal AgentsClotrimazole 1% cream5 g intravaginally daily for 7–14 daysClotrimazole 1% cream
Tradename:Recommended Regimens: Over-the-Counter Intravaginal AgentsClotrimazole 2% cream5 g intravaginally daily for 3 daysClotrimazole 2% cream
Tradename:Recommended Regimens: Over-the-Counter Intravaginal AgentsMiconazole 2% cream5 g intravaginally daily for 7 daysMiconazole 2% cream
Tradename:MonistatRecommended Regimens: Over-the-Counter Intravaginal AgentsMiconazole 4% cream5 g intravaginally daily for 3 daysMiconazole 4% cream
Tradename:Recommended Regimens: Over-the-Counter Intravaginal AgentsMiconazole 100 mg vaginal supositoryone suppository daily for 7 daysMiconazole 100 mg vaginal supository
Tradename:Monistat 7Recommended Regimens: Over-the-Counter Intravaginal AgentsMiconazole 200 mg vaginal suppositoryone suppository daily for 3 daysMiconazole 200 mg vaginal suppository
Tradename:Monistat 3Recommended Regimens: Over-the-Counter Intravaginal AgentsMiconazole 1,200 mg vaginal suppositoryone suppository for 1 dayMiconazole 1,200 mg vaginal suppository
Tradename:Monistat 1Recommended Regimens: Over-the-Counter Intravaginal AgentsTioconazole 6.5% ointment5 g intravaginally in a single applicationTioconazole 6.5% ointment
Tradename:Vagistat-1Recommended Regimens: Prescription Intravaginal AgentsButoconazole 2% cream (single dose bioadhesive product)5 g intravaginally in a single applicationButoconazole 2% cream (single dose bioadhesive product)
Tradename:GynazoleRecommended Regimens: Prescription Intravaginal AgentsTerconazole 0.4% cream5 g intravaginally daily for 7 daysTerconazole 0.4% cream
Tradename:Terazol 7Recommended Regimens: Prescription Intravaginal AgentsTerconazole 0.8% cream5 g intravaginally daily for 3 daysTerconazole 0.8% cream
Tradename:Terazol 3Recommended Regimens: Prescription Intravaginal AgentsTerconazole 80 mg vaginal suppositoryone suppository daily for 3 daysTerconazole 80 mg vaginal suppository
Tradename:Terazol 3 SuppositoryRecommended Regimen: Oral AgentFluconazole150 mg orally in a single doseFluconazole
Tradename:DiflucanNote: the creams and suppositories in these regimens are oil based and might weaken latex condoms and diaphragms. Patients should refer to condom product labeling for further information.Source: Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. Diseases characterized by vaginal itching, burning, irritation, odor or discharge: vulvovaginal candidiasis. MMWR Recomm Rep. 2021;70(No. RR-4):1-187. [2021 STI Treatment Guidelines]Share by e-mail
Check
-On-
Learning
QuestionsThe Check-on-Learning Questions are short and topic related. They are meant to help you stay on track throughout each lesson and check your understanding of key concepts.You must be signed in to customize your interaction with these questions.
Since you've received 80% or better on this quiz, you may claim continuing education credit.
You seem to have a popup blocker enabled. If you want to skip this dialog please Always allow popup windows for the online course.
Current Version: nstdc-monorepo-0406a550-2025-04-04-232359Become a New UserAccount Registration Benefits:
- Track your progress on the 9 lessons
- Earn free CNE/CME/CE
- Earn Certificates of Completion
- Access to other free IDEA curricula
Create a free account to get started
- 0%Lesson 2